Latest Posts
Guest Blog Post At Healthcare Law Blog: Straight Jackets For Everyone Over Age 65
 Thanks to my friend and fellow blogger Bob Coffield for hosting me (during my homeless period) at the Healthcare Law Blog. Here is an excerpt of my post:
Thanks to my friend and fellow blogger Bob Coffield for hosting me (during my homeless period) at the Healthcare Law Blog. Here is an excerpt of my post:
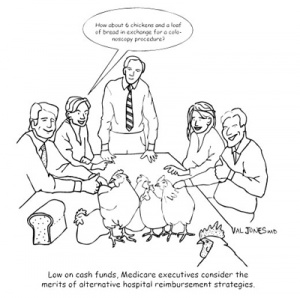
Today I viewed a TV ad sponsored by the AARP. It was promoting a remote alarm device that elderly people could use to notify EMS if they fall and need help. The ad featured a surprising statistic:“One in three people over the age of 65 will fall down this year.”That’s a pretty common occurrence, wouldn’t you say? It certainly argues for the need for those wearable alarm buttons.But at the same time that these ads are running on television, Medicare is moving forward with their “never event” quality program. The initiative means that Medicare will not pay for the care of patients who experience a “never event” in a hospital – funding for that patient’s care will need to come out of the hospital’s budget. Medicare argues that they shouldn’t have to pay for medical errors such as “wrong side surgery.”While I’m sympathetic to their perspective on wrong side surgery, the list of never events reaches far beyond the limits of medical errors to include things like mental status changes, infections and…drum roll please . . .Falls….
Will Cutting Doctor Salaries Improve Healthcare’s Bottom Line?
My friend and fellow blogger Dr. Kevin Pho just published an op-ed in USA Today explaining why cutting physician salaries will not reduce healthcare spending. Here is an excerpt:
The number of physicians who do not accept new Medicare patients is dramatic; in states like Texas, this number can exceed 40%. No wonder, as Medicare pays less than half of doctors’ fees. This scenario comes as a record number of Boomers approach Medicare age.
Those without Medicare are not spared the consequences. Seniors sometimes delay their care, leading to expensive treatment in the emergency department. Doctors who lose money seeing Medicare patients could pass on the costs to the privately insured.
According to the Kaiser Family Foundation, there are more significant drivers of health costs, including new prescription drugs, technology and administrative needs. Princeton economist Uwe Reinhardt estimates that physicians’ take-home pay represents roughly 10% of national health care spending. Cutting physician pay by 20% would only reduce spending by 2%.
I’ve also blogged about the plight of primary care physicians – as their salaries do not allow them to meet their high overhead costs.
As decreases in Medicare reimbursements begin to make it impossible for small practices to afford their supplies, rent, and coding and billing staff, more physicians will simply stop accepting Medicare patients. This means that the taxes that Baby Boomers have been paying all their lives will essentially not result in a guarantee of good medical coverage in their retirement. They may need to pay out-of-pocket to purchase additional insurance or to have a good primary care physician available to them 24-7.
Concierge practices like Alan Dappen’s may fill a gap in care. With full price transparency, availability via email and phone 24 hours a day, 7 days a week, house calls, and affordable fees – savvy patients will realize that his services are well worth the small out-of-pocket expense (on average, his patients spend $300/year on his services).
What’s my bottom line? I think we all need to save as much as we can of our own personal funds in case government programs do not provide us with adequate health coverage in our futures. At least if we grow our own healthcare nest egg, we’ll have more care choices in the future. And those choices may one day be a matter of life and death.
This post originally appeared on Dr. Val’s blog at RevolutionHealth.com.
Can Infections Be Prevented In The Hospital Setting?
No one wants to become infected during their hospital stay. Unfortunately it’s not possible to guarantee that it won’t happen. Bacteria are everywhere. We carry them on our skin, in our bodies (especially our digestive tract), and they live in food, clothing, and anything we touch. When we undergo surgery, we cut through the skin/blood barrier that keep the bacteria out, making us vulnerable to inadvertent invasion.
There are ways to reduce the risk of infection (sterile surgical technique, appropriate wound care, and personal hygiene) but the risk is not zero. For the risk to be zero, one would have to begin with a “sterile” patient – a patient who carries no bacteria on or in their body. Since that will never happen, I’m afraid that hospital acquired infections are here to stay.
However, with government-sponsored health insurance programs on the brink of bankruptcy, decreasing expenditures is a high priority. Therefore, Medicare is suggesting that there are certain events that should never happen in the hospital and that they will no longer compensate hospitals for care associated with these events. Although I certainly agree that operating on the wrong body part is appropriately classified as a “never event,” the list has become so long that it includes things that cannot possibly be prevented in all cases (things like catching a cold, developing a blood clot, falling, or becoming infected).
What will result from listing infections as a “never event?” Will it encourage hospitals to improve their infection control processes? Maybe. But here’s what I imagine is more likely to happen:
1. More prophylactic antibiotics will be given to patients to reduce the risk of infection, resulting in higher rates of serious drug reactions. Stronger medicine (with broader coverage) will be preferentially selected – further encouraging the development of drug resistant strains of bacteria.
2. Patients who become infected will be transferred to another facility as quickly as possible. The accepting facility will be compensated for the care of the patient since the “never event” didn’t happen at their hospital. Transferring care in the middle of a serious illness increases the risk for other complications, including miscommunications and medication errors.
3. Since Medicare has set the expectation that hospital acquired infections are 100% preventable, anyone who contracts one will be able to sue the hospital. This will deplete the hospitals of their thin operating margins, causing them to cut programs – probably first for the poor and underserved.
4. Additional testing may be done for any surgical admission – nasal swabs (and potentially rectal swabs or urethral swabs) will be used to document the fact that the patient arrived at the hospital colonized by certain bacteria and therefore did not contract a new infection during their hospital stay.
5. Convoluted documentation methods will abound, so that any patient who becomes infected will receive antibiotics for “prophylaxis” and his fevers will be explained as the usual “post-op” central fevers. All staff will be encouraged to carefully document that the patient is being treated prophylactically only, and does not have an infection. In fact, it’s possible that blood cultures will not be drawn so that there will be no documentation of sepsis. Patients who really do have serious infections will receive appropriate care very late (since the first few days will be spent trying to manage the infection without documenting it or identifying the organism). This could paradoxically result in higher death rates.
6. Patients at higher risk for infection (such as those who are immunocompromised – see my research study on risk factors for line infections here) may be passed over for surgical procedures. This risk aversion could negatively impact health outcomes for vulnerable populations (such as cancer patients or HIV+ individuals).
I could go on theorizing, but you get the picture. In my opinion, the “never events” strategy is fatally flawed and will result in excessive litigation, ping-ponging of patient care, over-use of antibiotics, increases in adverse drug events, a rise in multi-drug resistant bacteria, and further reduction of services to the poor. A more reasonable approach would have been to document infection rates at the most hygienic facilities, and offer incentives for others to strive for similar rates.
The “never events” strategy is destined to do more harm than good for patients with hospital acquired infections, though the medical malpractice attorneys may enjoy a new income stream. This is just one more reason why we should never say never.
***
See Buckeye Surgeon’s take on this topic and his coverage of Jerome Groopman’s article for the New Yorker on the rise of drug resistant “super bugs.”
See Dr. Rich’s take on never events here.This post originally appeared on Dr. Val’s blog at RevolutionHealth.com.
What Would The Ideal Health IT System Look Like?
I recently interviewed former Congresswoman Nancy Johnson about her views on health information technology (IT). She described her vision of an ideal IT solution, and what it should be able to do for physicians and patients. For the full interview, please check out my post at Medpolitics.com
Dr. Val: What would the ideal IT system look like?
Ms. Johnson: It would offer continuously updated evidence-based guidelines at the point of care for physicians. It would give patients clear information about what they should expect. It would enable physician social networks to promote learning and experience sharing with one another. It would promote continuous improvement of care practices, and track outcomes and results to continue refining healthcare delivery. Patients should be given check lists and preventive health guidelines, and be asked to provide feedback on any complications or unanticipated events.
If we could aggregrate deidentified patient information we would gain powerful insight into adverse drug events (or unanticipated positive effects) at the very earliest stages. It could be useful in identifying and monitoring epidemics or even terrorist incidents. This could advance medical science faster than ever before. Until we have all this information at our finger tips, we can’t imagine all the potential applications.
Dr. Val: Are you describing a centralized, national EMR?
Ms. Johnson: Not necessarily. But if systems are interoperable, it could function as one. I imagine it as a series of banks run by local administrators, but with the capability of sharing certain deidentified data with one another.
Dr. Val: Do you think the government should design this information system?
Ms. Johnson: No. You don’t want the government doing it alone. As much as I love the government and have been working in it for decades, it’s simply not good at updating and modernizing systems. You have to have a public-private partnership in this. The government should be involved to protect the public interest, and the private sector should be involved so that the system can be innovative, nimble, and easily updated.
Technology will bring us extraordinary new capabilities to manage our health, prevent illness, minimize the impact of disease on our lives, improve the ability of physicians to evaluate our state of health, allow us to integrate advances in medicine in a timely fashion, and quantify the impact of new inventions and procedures. All this, and IT will help us to promote prevention and control costs associated with acute care.
We have a high quality system now, but because it’s so disorganized, the patient doesn’t receive the quality they should. The incredible advances in technology that we have created should be available to all who need it. Unfortunately that’s not the case now.
If you look at Canada’s use of the specialist and specialist equipment along the US’s border with Canada, it says a lot about government run healthcare.
*See full interview at Medpolitics.com*This post originally appeared on Dr. Val’s blog at RevolutionHealth.com.