January 26th, 2011 by RamonaBatesMD in Better Health Network, Research
No Comments »

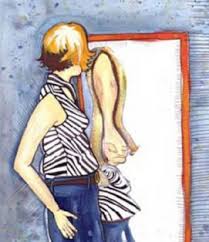 The Science Daily article entitled Body dysmorphic disorder patients who loathe appearance often get better, but it could take years discusses the disorder as highlighted in the Journal of Nervous and Mental Disease (JNMD).
The Science Daily article entitled Body dysmorphic disorder patients who loathe appearance often get better, but it could take years discusses the disorder as highlighted in the Journal of Nervous and Mental Disease (JNMD).
The JNMD article reports the results of the longest-term study so far to track people with body dysmorphic disorder (BDD). The study was conducted by researchers at Brown University and Rhode Island Hospital. The good news? The researchers “found high rates of recovery, although recovery can take more than five years.”
This is a small study with only 15 BDD patients who were followed over an eight-year span. An excerpt:
After statistical adjustments, the recovery rate for sufferers in the study over eight years was 76 percent and the recurrence rate was 14 percent. While a few sufferers recovered within two years, only about half had recovered after five years.
The subjects were a small group diagnosed with the disorder out of hundreds of people participating in the Harvard/Brown Anxiety Research Project (HARP). Study co-author Martin Keller, professor of psychiatry and human behavior and principal investigator of the HARP research program which has been ongoing for more than 20 years, said that because the BDD sufferers were identified through this broader anxiety study, rather than being recruited specifically because they had been diagnosed with BDD, they generally had more subtle cases of the disorder than people in other BDD studies. In comparing the HARP study with the prior longitudinal study of BDD, it is possible that the high recovery rate in the HARP study is due to participants having less severe BDD on average.
About body dysmorphic disorder:
— In its simplest definition, it is an obsessive preoccupation with a slight, imperceptible, or actually nonexistent anatomic irregularity to the degree that it interferes with normal adjustment within society. Read more »
*This blog post was originally published at Suture for a Living*
January 16th, 2011 by Dinah Miller, M.D. in Better Health Network, Opinion
No Comments »


 I’ve followed in bits and pieces — sometimes for Shrink Rap, sometimes because the issues fill my email inbox, sometimes because there’s no escape. Oh, and lots of the players have familiar names.
I’ve followed in bits and pieces — sometimes for Shrink Rap, sometimes because the issues fill my email inbox, sometimes because there’s no escape. Oh, and lots of the players have familiar names.
In the December 27th issue of Wired magazine, Gary Greenberg writes a comprehensive article on the debates around the revision of the American Psychiatric Association’s (APA) upcoming revision of the Diagnostic and Statistical Manual (DSM) entitled “Inside the Battle to Define Mental Illness.” Do read it. Here’s an excerpt:
I recently asked a former president of the APA how he used the DSM in his daily work. He told me his secretary had just asked him for a diagnosis on a patient he’d been seeing for a couple of months so that she could bill the insurance company. “I hadn’t really formulated it,” he told me. He consulted the DSM-IV and concluded that the patient had obsessive-compulsive disorder.
“Did it change the way you treated her?” I asked, noting that he’d worked with her for quite a while without naming what she had.
“No.”
“So what would you say was the value of the diagnosis?”
“I got paid.” Read more »
*This blog post was originally published at Shrink Rap*
January 13th, 2011 by Michael Craig Miller, M.D. in Health Policy, News
1 Comment »

When reports arrived that accused gunman Jared Lee Loughner had opened fire in Tucson, Arizona on January 7, journalistic first responders linked the incident to the fierceness of political rhetoric in the United States. Upon reflection, some of the discussion has turned to questions about mental illness, guns, and violence.
And plenty of reflection is required, because the connections are not at all simple. To get a sense of just how complicated they are, we invite you to read the lead article in this month’s Harvard Mental Health Letter entitled, “Mental Illness and Violence.” Strangely (for us) it was prepared for publication a month before the tragedy in Tucson. In light of the shooting, we are making the article available to non-subscribers.
I am not surprised at the outrage expressed in the news or at the impulse to blame. A quick scan of the news, however, shows there is not much agreement about whom to blame. In addition to the alleged perpetrator, one can find explicit and implicit criticisms of politicians for playing to our baser instincts; of media figures, various men and women of zeal, for their disingenuous or manipulative partisanship; of the various community bystanders (police, teachers, doctors, family members, neighbors, friends), whom we imagine could have intervened to prevent tragedy.
The political debate flowing from this incident will continue, as will the endless cycle of blame and defensiveness. But I caution all of us — and especially mental health professionals — not to make clinical judgments about Mr. Loughner. Very few people will or should have access to the kind of information that would allow such judgments. From a public health perspective, however, we should make careful judgments about policies that could reduce risk. Read more »
*This blog post was originally published at Harvard Health Blog*
January 5th, 2011 by AnneHansonMD in Better Health Network, Humor, News, Research
No Comments »



 I was surfing around the Net one day and I found this article about scientists who are creating a machine that will detect acetone in someone’s breath. Acetone can be a sign that someone suffers from diabetes, so in theory this machine could use scent to diagnose this disease.
I was surfing around the Net one day and I found this article about scientists who are creating a machine that will detect acetone in someone’s breath. Acetone can be a sign that someone suffers from diabetes, so in theory this machine could use scent to diagnose this disease.
That story brought to mind other stories I’ve heard about people using dogs to sniff out cancer in people. According to this article:
“The results of the study showed that dogs can detect breast and lung cancer with sensitivity and specificity between 88% and 97%. The high accuracy persisted even after results were adjusted to take into account whether the lung cancer patients were currently smokers. Moreover, the study also confirmed that the trained dogs could even detect the early stages of lung cancer, as well as early breast cancer.”
People have even tried “smelling” schizophrenia. Read more »
*This blog post was originally published at Shrink Rap*
December 26th, 2010 by Glenn Laffel, M.D., Ph.D. in Better Health Network, Health Tips, News, Research
3 Comments »

 Flashbacks are vivid, recurring, intrusive, and unwanted mental images of a past traumatic experience. They are a sine qua non of post-traumatic stress disorder (PTSD). Although drugs and cognitive behavioral interventions are available to treat PTSD, clinicians would prefer to utilize some sort of early intervention to prevent flashbacks from developing in the first place.
Flashbacks are vivid, recurring, intrusive, and unwanted mental images of a past traumatic experience. They are a sine qua non of post-traumatic stress disorder (PTSD). Although drugs and cognitive behavioral interventions are available to treat PTSD, clinicians would prefer to utilize some sort of early intervention to prevent flashbacks from developing in the first place.
Well, researchers at Oxford University appear to have found one. Remarkably, all it takes is playing Tetris. Yes, Tetris!
The team responsible for the discovery was led by Emily Holmes. The writeup appears in the November issue of PLoS ONE. Holmes and colleagues had reasoned that the human brain has a limited capacity to process memories, and that memory consolidation following a traumatic experience is typically complete within six hours after the event. Holmes’ team also knew that playing Tetris involved the same kind of mental processing as that involved with flashback formation. So they figured if they had people play Tetris during that six-hour window after the traumatic event, it might interfere with memory consolidation of the traumatic experience. That, in turn, would reduce or eliminate the flashbacks. The idea worked like a charm. Read more »
*This blog post was originally published at Pizaazz*
The Science Daily article entitled Body dysmorphic disorder patients who loathe appearance often get better, but it could take years discusses the disorder as highlighted in the Journal of Nervous and Mental Disease (JNMD).





 I’ve followed in bits and pieces — sometimes for Shrink Rap, sometimes because the issues fill my email inbox, sometimes because there’s no escape. Oh, and lots of the players have familiar names.
I’ve followed in bits and pieces — sometimes for Shrink Rap, sometimes because the issues fill my email inbox, sometimes because there’s no escape. Oh, and lots of the players have familiar names.











