November 26th, 2012 by Dr. Val Jones in Health Tips, Opinion, Research
5 Comments »
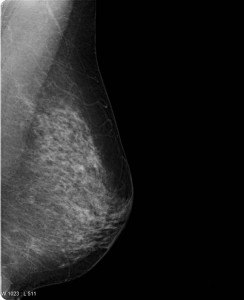 A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A question on most women’s minds (as they turn 40 and beyond) is whether or not they should get a screening mammogram (x-ray of the breasts). If you have found a lump in your breast or you have a family history of breast cancer the answer is yes. No need to read any further. However, for the majority of us lumpless, family-history-free women, a screening mammogram is far more likely to expose us to unnecessary follow up testing than it is to catch a tumor early. Dr. Welch explains that screening mammograms aren’t very good at identifying aggressive breast cancer early enough to make a difference in whether one lives or dies anyway. That’s very disappointing news.
Dr. Welch goes on to explain that most of the gains we’ve made in breast cancer survival have been because of improved breast cancer treatments, not because of early detection with mammograms. He estimates that every year in the U.S. 1.3 million women are “over-diagnosed” with breast cancer because of screening mammograms, subjecting women to unnecessary biopsies, surgical procedures, and further follow up studies. In the video, Dr. Welch doesn’t explain exactly what these “over diagnosed” cancers end up being exactly (Cysts? Benign calcifications? Early non-aggressive cancers that the immune system kills on its own?) But suffice it to say that they don’t contribute to the cancer death rates.
So, given the fact that you are more likely to suffer through a false alarm than to discover a cancer early (and even if you do find it early, if it’s the “bad” kind you may not survive) are you willing to undergo a screening mammogram? That’s a personal question that we each have to answer for ourselves. As time goes on, however, I suspect that the answer will be made for us since health insurance companies (whether public or private) will begin to balk at paying for tests that do more harm than good overall. I think this issue is really at the heart of the controversy (the perception of rolling back a health benefit that women currently “enjoy”). Eventually screening mammograms may become an out-of-pocket expense for women who simply prefer the peace of mind that a normal test can give – even at the risk of going through a false alarm.
That being said, it sure would be great if we could find a screening test that identifies breast cancer early – especially the aggressive kind. Perhaps a blood test will do the trick one day? At least it is comforting to know that we have made great strides on the treatment side, so that fewer women than ever before die of breast cancer. More research is needed on both the screening and treatment sides of course.
As for me, I do regular breast self exams – though because I have no family history of breast cancer I’ve opted out of screening mammograms because I feel the cost/benefit ratio is not in my favor. I certainly hope that a better screening test is developed before I face a potential diagnosis. I respect that other women will disagree with me – and I think they have the right to be screened with the only option we currently have: the mammogram. I’m not sure how long it will continue to be covered by insurance, but at a price point of about $100, most of us could still afford to pay for it out-of-pocket if desired.
The bottom line of this controversial research study is that screening mammograms don’t actually catch death-causing breast cancers early enough to alter their course. Even though it makes intuitive sense to be screened, long term observations confirm that overall, mammograms do more harm than good. So now we wait for a better test – while some of us continue with the old one (as the National Cancer Institute recommends), and others (like me) don’t bother.
***
Thanks to ePatient Dave and Susannah Fox who brought the issue to my attention on Facebook. Isn’t social media grand?
December 27th, 2011 by GruntDoc in Health Policy, Opinion
No Comments »

This article and its graph (from the NEJM), and its interesting, informative but probably useless graph, was referenced today on twitter, via the Washington Post’s Wonkblog,
Recently, the Centers for Medicaid and Medicare Services announced a scheduled cut in Medicare physician fees of 27.4% for 2012. This cut stems from the sustainable growth rate (SGR) formula used by the physician-payment system. …
To illustrate the level of inequity in this system, we broke down the national spending for Medicare physician services by state and by specialty and determined which states and specialties have contributed most to the SGR deficit between 2002, when the program was last balanced, and 2009. Although SGR spending targets are set on a national level, we computed state targets by applying the SGR’s national target growth rate to each state’s per capita expenditure, using 2002 as the base year. Our analysis is an approximation, because, unlike the SGR, we do not adjust for differential fee changes. …
We compared the state targets for the years 2003 to 2009 to actual state expenditures and added the annual difference between these figures to get a cumulative difference between the state’s spending and the SGR target. This cumulative difference was Read more »
*This blog post was originally published at GruntDoc*
December 4th, 2011 by DavedeBronkart in News, Research
1 Comment »

 Wow. Todd Park, Chief Technical Officer at HHS, ought to be jumping out of his skin with joy at this one.
Wow. Todd Park, Chief Technical Officer at HHS, ought to be jumping out of his skin with joy at this one.
This time, House, M.D. fans, it was lupus. The article “Evidence-Based Medicine in the EMR Era” published in the Nov. 10 issue of the New England Journal of Medicine might have read like a House television script, but it was a real-life glimpse of what the most optimistic health IT advocates are hoping will become commonplace in U.S. health care: Mining EHR data to arrive at treatment decisions.
 In a Health IT Exchange piece (on TechTarget) EHR data spurs real-time evidence-based medicine, Don Fluckinger summarizes (and dramatizes, accurately) this early specimen of care being transformed – beyond the literature – by looking at past records. Faced with a 13 year old lupus patient with a complex problem (see article for details)…
In a Health IT Exchange piece (on TechTarget) EHR data spurs real-time evidence-based medicine, Don Fluckinger summarizes (and dramatizes, accurately) this early specimen of care being transformed – beyond the literature – by looking at past records. Faced with a 13 year old lupus patient with a complex problem (see article for details)…
In four hours, they did a retrospective study of similar patients in the hospital’s data warehouse…, and decided to move ahead with the treatment based on the previous results of 98 [similar patients] … The authors said they will never know if they made the “correct” decision, but they did know that — in absence of randomized trial research to support their decision — they acted on the evidence of the best data available, coupled with their experience.
“Our case is but one example of a situation in which the existing literature is insufficient to guide the clinical care of a patient,” the authors wrote. …
What are we waiting for, people?? Imagine if Read more »
*This blog post was originally published at e-Patients.net*
August 28th, 2011 by Michael Kirsch, M.D. in Opinion, Research
No Comments »

 Medical malpractice reform is in the news again. Of course, for the medical profession, the medical malpractice system is the wound that simply will not heal. For the plaintiffs bar, in contrast, the medical liability system is the gift that keeps on giving. I have argued that the current system fails on four important fronts.
Medical malpractice reform is in the news again. Of course, for the medical profession, the medical malpractice system is the wound that simply will not heal. For the plaintiffs bar, in contrast, the medical liability system is the gift that keeps on giving. I have argued that the current system fails on four important fronts.
- Efficiency
- Cost
- Fairness
- Quality Improvement
I admit readily that my profession has not been as diligent as it should be in holding ourselves accountable. We have not been forthright in admitting our medical errors, although can you blame us under the current medical liability construct? Read more »
*This blog post was originally published at MD Whistleblower*
August 20th, 2011 by Paul Auerbach, M.D. in Research
1 Comment »

 Yellow fever is an affliction caused by a potentially lethal viral (flavivirus) hemorrhagic (causes bleeding) virus common in parts of Africa and South America. A highly effective vaccine made from live virus (known as the “17D vaccine”) is currently used to inject persons to prevent yellow fever; this vaccine is known to rarely cause serious adverse effects, namely, onset of allergic reactions, or a life-threatening or fatal infection that resembles yellow fever.
Yellow fever is an affliction caused by a potentially lethal viral (flavivirus) hemorrhagic (causes bleeding) virus common in parts of Africa and South America. A highly effective vaccine made from live virus (known as the “17D vaccine”) is currently used to inject persons to prevent yellow fever; this vaccine is known to rarely cause serious adverse effects, namely, onset of allergic reactions, or a life-threatening or fatal infection that resembles yellow fever.
So, there is need for a safer (“nonreplicating”—in other words, not based on live virus) vaccine. In a recent article, “An Inactivated Cell-Culture Vaccine against Yellow Fever,” Thomas Monath, MD and his coauthors described their experience with a potentially safer vaccine (NEJM, 2011;364:1326-33). In their study, Read more »
This post, Advancement In Research For A Safer Yellow Fever Vaccine, was originally published on
Healthine.com by Paul Auerbach, M.D..
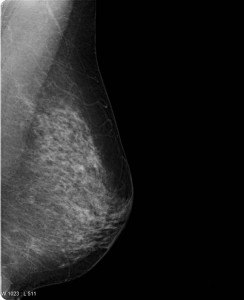 A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.







 Yellow fever is an affliction caused by a potentially lethal viral (flavivirus) hemorrhagic (causes bleeding) virus common in parts of Africa and South America. A highly effective vaccine made from live virus (known as the “17D vaccine”) is currently used to inject persons to prevent yellow fever; this vaccine is known to rarely cause serious adverse effects, namely, onset of allergic reactions, or a life-threatening or fatal infection that resembles yellow fever.
Yellow fever is an affliction caused by a potentially lethal viral (flavivirus) hemorrhagic (causes bleeding) virus common in parts of Africa and South America. A highly effective vaccine made from live virus (known as the “17D vaccine”) is currently used to inject persons to prevent yellow fever; this vaccine is known to rarely cause serious adverse effects, namely, onset of allergic reactions, or a life-threatening or fatal infection that resembles yellow fever.







