May 18th, 2011 by Medgadget in Health Tips, News
1 Comment »

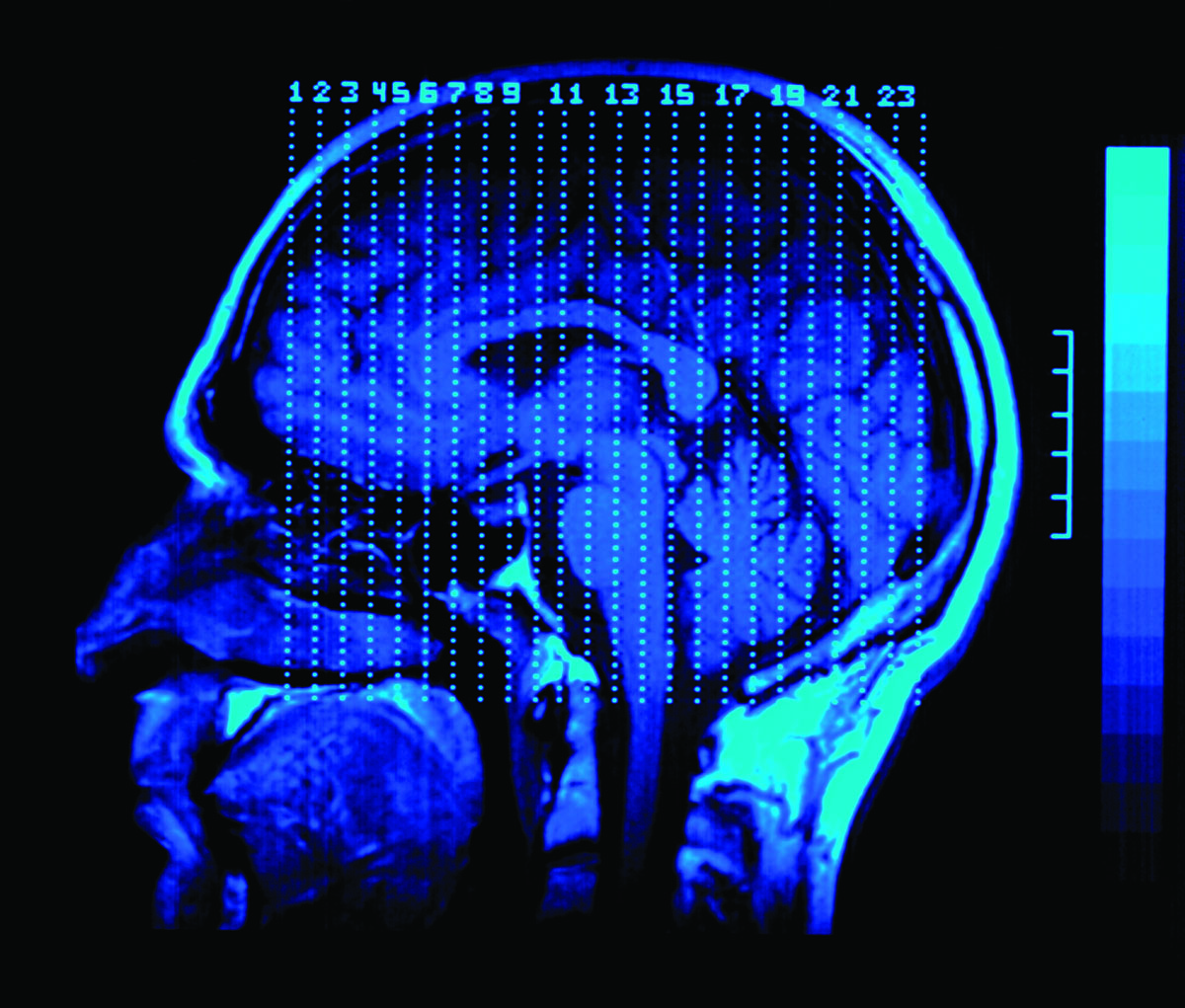
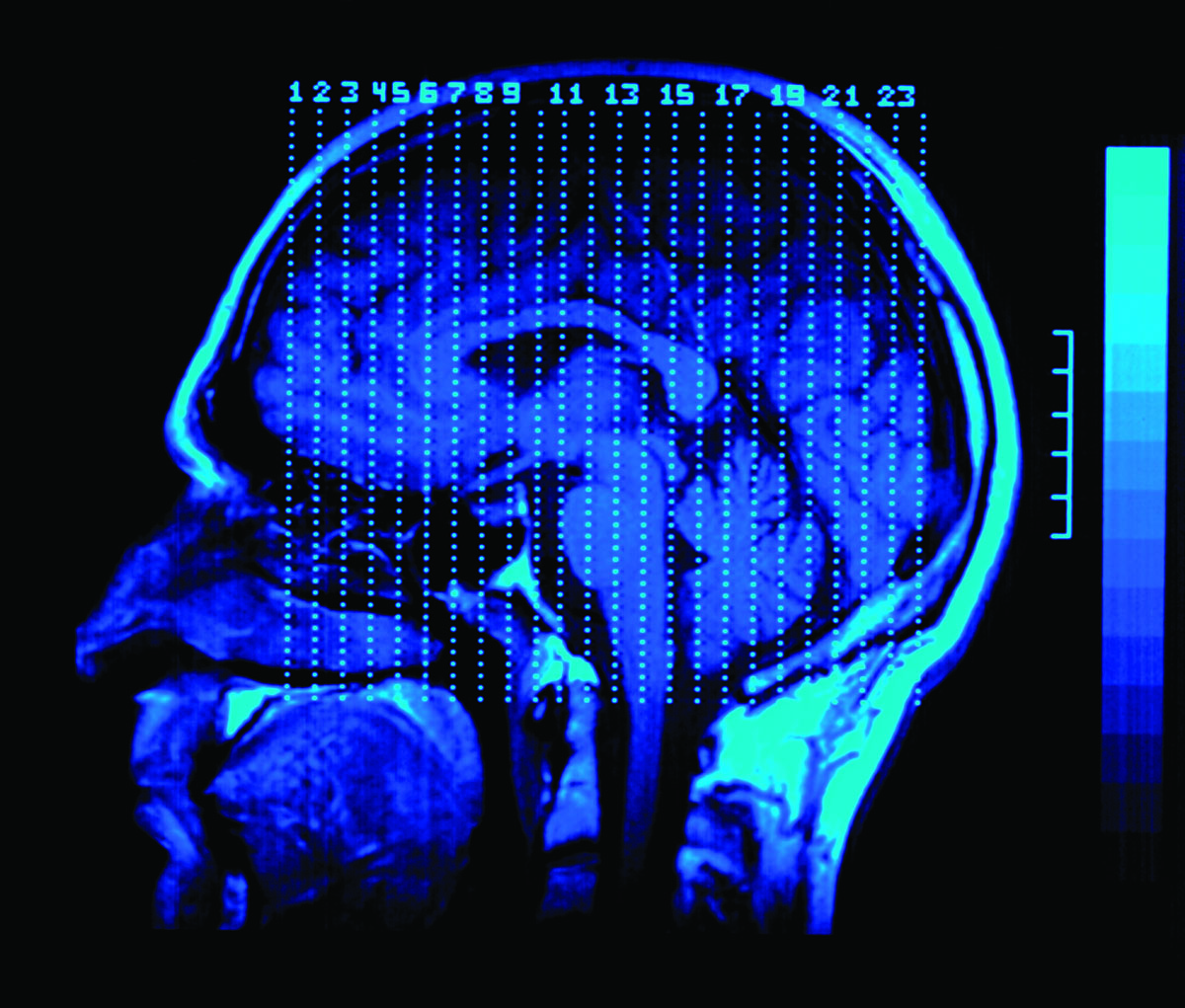
 Researchers from the University of Calgary have shown that doctors can make a stroke diagnosis using an iPhone application just as accurately (and faster) than they can on a traditional computer. In a study recently published by Journal of Medical Internet Research, two neuro-radiologists looked at 120 consecutive noncontrast computed tomography (NCCT) scans and 70 computed tomography angiogram (CTA) head scans. One used a diagnostic workstation and the other using Calgary Scientific‘s ResolutionMD Mobile app. The study results showed that using the ResolutionMD app is between 94%-100% accurate in diagnosing acute stroke, compared to a medical workstation.
Researchers from the University of Calgary have shown that doctors can make a stroke diagnosis using an iPhone application just as accurately (and faster) than they can on a traditional computer. In a study recently published by Journal of Medical Internet Research, two neuro-radiologists looked at 120 consecutive noncontrast computed tomography (NCCT) scans and 70 computed tomography angiogram (CTA) head scans. One used a diagnostic workstation and the other using Calgary Scientific‘s ResolutionMD Mobile app. The study results showed that using the ResolutionMD app is between 94%-100% accurate in diagnosing acute stroke, compared to a medical workstation.
In addition to accurately diagnosing a stroke, the app was also praised for its ability to handle a large number of images seamlessly and to detect subtle, but potentially critical findings in CT scans. Moreover, the mobile nature of the app gives doctors the ability to analyze and diagnose strokes from practically anywhere. Read more »
*This blog post was originally published at Medgadget*
May 10th, 2011 by RyanDuBosar in News
No Comments »

About 9% of infants are given dietary botanical supplements or teas as young as 1 month old, prompting government researchers to warn physicians to look for side effects and other health risks.
Supplement use is common. Parents use them to help with fussiness, digestion, colic, and relaxation. Parents like them because there’s no prescription required, they’re traditional to many cultures, and they’re marketed as “natural.”
But, caution the authors of a paper that appeared in the journal Pediatrics, such supplements’ purity and potency are unregulated, they can interact with prescription medicines, they may contain heavy metals or other contaminants, and they may not adapt well to a newborn’s metabolism and body weight.
Supplement use is also common as a cause of emergency room visits. And they’re linked to seizures and death.
Researchers from the Food and Drug Administration and the Centers for Disease Control and Prevention used data from the Infant Feeding Practices Study II, a longitudinal survey of 2,653 women studied from late pregnancy through the first year of the child’s life. The sample was drawn from a nationally distributed consumer opinion panel of healthy adult mothers with healthy term or near-term infants.
*This blog post was originally published at ACP Internist*
May 7th, 2011 by Happy Hospitalist in Opinion
No Comments »

 So I’m rounding in the ICU the other day when I came upon this new hospital medical device. It’s called a pupillometer. What does this pupillometer do? It measures subtle changes in the light reflex of the pupil to help take the physical exam to the next level of precision.
So I’m rounding in the ICU the other day when I came upon this new hospital medical device. It’s called a pupillometer. What does this pupillometer do? It measures subtle changes in the light reflex of the pupil to help take the physical exam to the next level of precision.
Or eliminate it, depending on how you look at it. What used to be a basic physical exam skill is now being replaced by a $6000 piece of medical technology that can distinguish tiny changes in pupil size. Now the real questions remain. Has this pupillometer device gone through the rigors of randomized trials in the ICU to define whether a $6000 flashlight changes outcomes or mortality? And if not, how do we allow medications to require such testing but not the technology that often changes nothing and simply makes health care more expensive.
The way I see things, if I’m trying to decide whether someone’s pupils constrict 1% vs 3% vs 10%, I’m getting a palliative care consult instead and putting the pupillometer back in my holster.
First the vein light. Now the pupillomter. And I thought the super bright LED pen light was all the rage.
*This blog post was originally published at The Happy Hospitalist*
May 2nd, 2011 by Glenn Laffel, M.D., Ph.D. in Health Policy, Opinion
1 Comment »


For the first time in 30 years, an expert panel has updated guidelines for the diagnosis of Alzheimer’s disease. The long overdue facelift should favorably impact care for millions and accelerate badly needed research on the disease.
The guidelines were produced by representatives from the National Institute on Aging and the Alzheimer’s Association. They portray Alzheimer’s for the first time as a three-stage disease. In addition to ‘Stage 3,’—the full-blown clinical syndrome that had been described in earlier versions of the guidelines—the new guidelines describe an earlier ‘Stage 2,’ of mild cognitive impairment due to Alzheimer’s, and a ‘Stage 1, or preclinical’ phase of the disease. The latter can only be detected with biochemical marker tests and brain scans.The guidelines legitimize years’ worth of observations by the family members of Alzheimer’s patients, who recognize in retrospect that Grandpa had a slowly progressive cognitive disorder long before he was diagnosed. The guidelines also reflect progress on the research front, where it has now been established that the disease begins years before patients become symptomatic.
Alzheimer’s patients and their families, and the teetering US health system that supports them, would have been better served by the publication of these guidelines 2-3 years ago. Read more »
*This blog post was originally published at Pizaazz*
March 31st, 2011 by admin in Health Policy, Health Tips, Research
No Comments »
By Richard C. Hunt, MD, FACEP
Centers for Disease Control and Prevention
A 17 year-old athlete arrives on the sideline, at your office, or in the emergency department after hitting her head during a collision on the sports field and is complaining that she has a headache and “just doesn’t feel right.”
Can she return to play? If not, when can she safely return to school, sports, and to her normal daily activities? Does she need immediate care, a Head CT or MRI, or just some time to rest?
Do those questions sound familiar?
Each year thousands of young athletes present at emergency departments and in the primary care setting with a suspected sports- and recreation-related concussion. And every day, health care professionals, like us, are challenged with identifying and appropriately managing patients who may be at risk for short- or long-term problems.
As you know, concussion symptoms may appear mild, but this injury can lead to significant, life-long impairment affecting an individual’s ability to function physically, cognitively, and psychologically. Thus, appropriate diagnosis, referral, and education are critical for helping young athletes with concussion achieve optimal recovery and to reduce or avoid significant sequelae.
And that’s where you come in. Health care professionals play a key role in helping to prevent concussion and in appropriately identifying, diagnosing, and managing it when it does occur. Health care professionals can also improve patient outcomes by implementing early management and appropriate referral.
As part of my work at CDC, and as a health care professional, I am committed to informing others about CDC’s resources to help with diagnosing and managing concussion. CDC collaborated with several organizations and leading experts to develop a clinical guideline and tools for the diagnosis and management of patients with concussion, including:
For more information about the diagnosis and management of concussion, please visit www.cdc.gov/Concussion/clinician.html.
Also, learn more about CDC’s TBI activities and join the conversation at: www.facebook.com/cdcheadsup.
 Researchers from the University of Calgary have shown that doctors can make a stroke diagnosis using an iPhone application just as accurately (and faster) than they can on a traditional computer. In a study recently published by Journal of Medical Internet Research, two neuro-radiologists looked at 120 consecutive noncontrast computed tomography (NCCT) scans and 70 computed tomography angiogram (CTA) head scans. One used a diagnostic workstation and the other using Calgary Scientific‘s ResolutionMD Mobile app. The study results showed that using the ResolutionMD app is between 94%-100% accurate in diagnosing acute stroke, compared to a medical workstation.
Researchers from the University of Calgary have shown that doctors can make a stroke diagnosis using an iPhone application just as accurately (and faster) than they can on a traditional computer. In a study recently published by Journal of Medical Internet Research, two neuro-radiologists looked at 120 consecutive noncontrast computed tomography (NCCT) scans and 70 computed tomography angiogram (CTA) head scans. One used a diagnostic workstation and the other using Calgary Scientific‘s ResolutionMD Mobile app. The study results showed that using the ResolutionMD app is between 94%-100% accurate in diagnosing acute stroke, compared to a medical workstation.