December 3rd, 2011 by PeterWehrwein in Research
1 Comment »

Some medications are well known for being risky, especially for older people. Certain antihistamines, barbiturates, muscle relaxants—take too much of them, or take them with certain other medications, and you can wind up in serious trouble (and possibly in the back of ambulance).
But researchers from the federal Centers for Disease Control and Prevention (CDC) and Emory University reported in this week’s New England Journal of Medicine that those high-risk medications are not the ones that most commonly put older Americans (ages 65 and older) in the hospital.
Warfarin is #1
Instead, they found that warfarin is the most common culprit. Warfarin (the brand-name version is called Coumadin) reduces the blood’s tendency to clot. Many older people take it to lower their risk of getting a stroke.
After warfarin, different Read more »
*This blog post was originally published at Harvard Health Blog*
November 27th, 2011 by HarvardHealth in Health Tips, Research
No Comments »

Good vibrations may work for dancing on the beach or for romance, but they don’t seem to do much to strengthen bones.
Results of a clinical trial published in the Annals of Internal Medicine showed that older women who stood on a vibrating platform for 20 minutes a day experienced just as much bone loss over the course of the year-long trial as women who didn’t use the platform.
The results are a disappointment for older women and men looking to strengthen their bones without exercising, not to mention to the companies that have sprung up to sell whole-body vibration platforms as an easy way to halt osteoporosis, the age-related loss of bone.
The idea behind whole-body vibration makes sense. Like walking, running, and other weight-bearing physical activities, whole-body vibration Read more »
*This blog post was originally published at Harvard Health Blog*
November 21st, 2011 by HarvardHealth in Health Tips
No Comments »

No matter how sick my grandmother got or what her doctors said, she refused to go to the hospital because she thought it was a dangerous place. To some degree, she was right. Although hospitals can be places of healing, hospital stays can have serious downsides, too.
One that has been getting a lot of attention lately is the development of delirium in people who are hospitalized. Delirium is a sudden change in mental status characterized by confusion, disorientation, altered states of consciousness (from hyperalert to unrousable), an inability to focus, and sometimes hallucinations. It’s the most common complication of hospitalization among older people.
We wrote about treating and preventing hospital delirium earlier this year in the Harvard Women’s Health Watch. In the New York Times “The New Old Age” blog, author Susan Seliger vividly describes her 85-year-old mother’s rapid descent into hospital delirium, and tips for preventing it.
Although delirium often recedes, it may have long-lasting aftereffects. Read more »
*This blog post was originally published at Harvard Health Blog*
October 24th, 2011 by BobDoherty in Health Policy
No Comments »

“HERE is the dirty little secret of health care in America for the elderly, the one group we all assume has universal coverage thanks to the 1965 Medicare law: what Medicare paid for then is no longer what recipients need or want today.”
So argues New York Times reporter Jane Gross in a provocative op-ed in last Sunday’s New York Times. She makes the case that too much of Medicare is going to medical treatments and drugs of little value to the elderly, and nearly nothing on long-term care, citing the case of her own family’s experience:
“In the case of my mother, who died at 88 in 2003, room and board in various assisted living communities, at $2,000 to $3,500 a month for seven years, was not paid for by Medicare. Yet neurosurgery, I later learned was not expected to be effective in her case, was fully reimbursed, along with two weeks of in-patient care. Her stay of two years at a nursing home, at $14,000 a month (yes, $14,000) was also not paid for by Medicare. Nor were Read more »
*This blog post was originally published at The ACP Advocate Blog by Bob Doherty*
December 26th, 2010 by Elaine Schattner, M.D. in Better Health Network, News, Opinion, Research
No Comments »

This evening, when I finished cleaning up the kitchen after our family dinner, I glanced at the current issue of the Economist. The cover features this headline: the Joy of Growing Old (or why life begins at 46). It’s a light read, as this so-influential magazine goes, but nice to contemplate if you’re, say, 50 years old and wondering about the future.
The article’s thesis is this: Although as people move towards old age they lose things they treasure — vitality, mental sharpness and looks — they also gain what people spend their lives pursuing: Happiness.
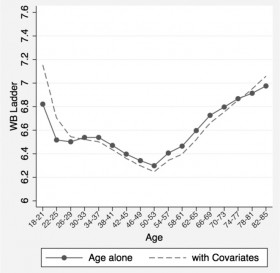
Fig. 1 (above): “A snapshot of the age distribution of psychological well-being in the United States,” Stone, et al: PNAS, May 2010 (y-axis: “WB” stands for well-being.)
Young adults are generally cheerful, according to the Economist’s mysterious author or authors. Things go downhill until midlife, and then they pick up again. There’s a long discussion in the article on possible reasons for the U-shaped curve of self-reported well-being. Most plausible among the explanations offered, which might be kind of sad except that in reality (as opposed to ideals) I think it’s generally a good thing, is the “death of ambition, birth of acceptance.” The concept is explained: “Maybe people come to accept their strengths and weaknesses, give up hoping to become chief executive or have a picture shown in the royal Academy…” And this yields contentedness. Read more »
*This blog post was originally published at Medical Lessons*