November 16th, 2011 by Jessie Gruman, Ph.D. in Opinion, Research
No Comments »


It is completely understandable if you associate the term “cancer survivor” with an image of glamorous, defiant Gloria Gaynor claiming that She. Will. Survive. Or maybe with a courageous Lance Armstrong in his quest to reclaim the Tour de France. Or perhaps it is linked for you with heroic rhetoric and pink-related racing, walking and shopping.

Phil Roeder from flickr.com
I never call myself a survivor because when I hear this term, I recall my experience following each of four cancer-related diagnoses. It has not been triumphant. It’s been terrifying and grueling. It hasn’t taken courage to get through the treatment. It’s taken doing the best I can. I am not still here because I am defiant. I am here because I am lucky, because I am cared for by good clinicians who treated my cancers based on the best available evidence, and because on the whole, I participated actively in my care. But mostly I am here because each successive diagnosis was made as a result of being followed closely with regular checks and screenings and because my doctors responded effectively to questionable findings and odd symptoms.
There are 12 million Americans living today who have been treated for cancer. Not only are we at risk for recurrences but, as Dr. Julia Rowland, director of the Office of Cancer Survivorship at the National Cancer Institute, notes, “Research shows that there are no benign therapies. All treatment is potentially toxic and some therapy may itself be carcinogenic. Today, people are living long enough to manifest the health consequences of efforts to cure or control their cancer.”
Who amongst our clinicians is responsible for helping us watch out for those consequences for the balance of our lives? Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
November 9th, 2011 by Lucy Hornstein, M.D. in Opinion
No Comments »

Cancer is a dreadful disease. Just dreadful. Make no mistake: I have tremendous respect for the awesome doctors who treat patients afflicted with it day after day. Still, paradoxically, I can’t help but notice that some of them have just as hard a time as do other doctors with caring for patients at the end of their lives. I believe a large part of their difficulty stems from the ridiculously dysfunctional either/or approach to palliative care and hospice we’re stuck with in this benighted country.
The problem is that in order to qualify for hospice, patients must not only have a certified life expectancy of less than six months, but they must also not be undergoing any active treatment for their malignancy. When you stop to think about it, though, this is actually quite discriminatory. We don’t require people on hospice with other diagnoses to discontinue their life sustaining medications. Patients with COPD are allowed to continue their bronchodilators; CHF patients don’t have to stop their ACE inhibitors and digoxin. But if a cancer patient wants to qualify for hospice, they have to forgo curative treatments like chemotherapy.
So what if the oncologists call it “palliative” chemo instead? Read more »
*This blog post was originally published at Musings of a Dinosaur*
October 26th, 2011 by MelissaSchaeferMD in Announcements, Health Tips
No Comments »

 As clinicians, we know that the nearly one million patients who receive outpatient cancer treatment each year are at risk for serious infections that may lead to hospitalization, disruptions in chemotherapy schedules, and in some cases, death. Even so, it appears that outpatient oncology facilities may vary greatly in their attention to infection prevention. As one example – at an oncology clinic in Nebraska, it was discovered that syringes were reused to access bags of saline that were shared among multiple patients. This unsafe practice led to the transmission of hepatitis C virus to at least 99 cancer patients, resulting in one of the largest healthcare-associated outbreaks of its kind.
As clinicians, we know that the nearly one million patients who receive outpatient cancer treatment each year are at risk for serious infections that may lead to hospitalization, disruptions in chemotherapy schedules, and in some cases, death. Even so, it appears that outpatient oncology facilities may vary greatly in their attention to infection prevention. As one example – at an oncology clinic in Nebraska, it was discovered that syringes were reused to access bags of saline that were shared among multiple patients. This unsafe practice led to the transmission of hepatitis C virus to at least 99 cancer patients, resulting in one of the largest healthcare-associated outbreaks of its kind.
To help address this problem, CDC is launching a new program called Preventing Infections in Cancer Patients, featuring tools to help both clinicians and patients prevent infections.
As a cornerstone of this new initiative, CDC worked with Read more »
*This blog post was originally published at Safe Healthcare*
October 19th, 2011 by AndrewSchorr in Health Policy, Interviews
No Comments »

If you’ve read my blogs for a while, or look up some past blogs, you’ll see I have been frustrated at times with the FDA. Yes, they have a tough job protecting us from medical products that are unsafe and/or ineffective. But when it comes to cancer, where we have few “homerun” therapies, I wish they were a bit more liberal. A “bunt single” might be good enough. You may have read how I have been critical of Dr. Rick Pazdur, the FDA leader for oncology drug approval. Some desperate patients and family members have referred to him as “Dr. No.”
Just the other day I interviewed a respected breast cancer survivor and patient advocate who has high respect for Dr. Pazdur. Musa Mayer of New York City is a 22-year breast cancer survivor and author of three books about breast cancer. She’s devoted her life to educating other patients about cancer and also playing a role in public policy. She has become a favorite patient representative on FDA cancer advisory boards and regularly weighs in when breast cancer drugs are being considered.
In my interview with Musa, she explained Read more »
*This blog post was originally published at Andrew's Blog*
October 16th, 2011 by Elaine Schattner, M.D. in Research
No Comments »

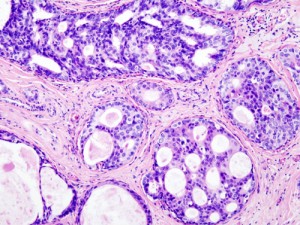
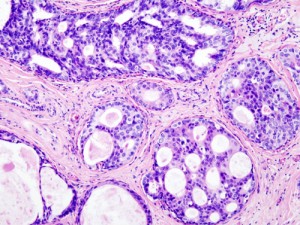
Ductal Carcinoma in Situ (DCIS) in the breast, histopathology w/ hematoxylin & eosin stain, Wiki-Commons image
More, a magazine “for women of style & substance,” has an unusually thorough, now-available article by Nancy F. Smith in its September issue on A Breast Cancer You May Not Need to Treat.
The article’s subject is DCIS (Ductal Carcinoma in Situ). This non-invasive, “Stage 0” malignancy of the breast has shot up in reported incidence over the past two decades. It’s one of the so-called slow-growing tumors detected by mammography; a woman can have DCIS without a mass or invasive breast cancer.
While some people with this diagnosis choose to have surgery, radiation or hormonal treatments, others opt for a watchful waiting strategy. The article quotes several physicians, including oncologists, who consider Read more »
*This blog post was originally published at Medical Lessons*







 As clinicians, we know that the nearly one million patients who receive outpatient cancer treatment each year are at risk for serious infections that may lead to hospitalization, disruptions in chemotherapy schedules, and in some cases, death. Even so, it appears that outpatient oncology facilities may vary greatly in their attention to infection prevention. As one example – at an oncology clinic in Nebraska, it was discovered that syringes were reused to access bags of saline that were shared among multiple patients. This unsafe practice led to the transmission of hepatitis C virus to at least 99 cancer patients, resulting in one of the largest healthcare-associated outbreaks of its kind.
As clinicians, we know that the nearly one million patients who receive outpatient cancer treatment each year are at risk for serious infections that may lead to hospitalization, disruptions in chemotherapy schedules, and in some cases, death. Even so, it appears that outpatient oncology facilities may vary greatly in their attention to infection prevention. As one example – at an oncology clinic in Nebraska, it was discovered that syringes were reused to access bags of saline that were shared among multiple patients. This unsafe practice led to the transmission of hepatitis C virus to at least 99 cancer patients, resulting in one of the largest healthcare-associated outbreaks of its kind.