March 9th, 2011 by AndrewSchorr in Better Health Network, Research, True Stories
No Comments »

Maybe you read the other day in The New York Times that the pharmaceutical industry has a problem. Big blockbuster drugs like Lipitor are going off patent and the industry leaders don’t have new blockbusters showing promise to replace them. So the big companies search for little companies with new discoveries and they consider buying them. Industry observers think the days of $5 billion-a-year drugs to lower cholesterol or control diabetes may be past for awhile, and the companies will have smaller hits with new compounds for autoimmune conditions and cancer.
When I saw my oncologist for a checkup yesterday — the news was good — we chatted about the article and the trend toward “niche science.” We welcomed it. We didn’t think — from our perspective — the world needed yet another drug to lower cholesterol. We need unique products to fight illnesses that remain daunting, some where there are no effective drugs at all. For example, my daughter has suffered for years from what seems to be an autoimmune condition called eosinophilic gastroenteritis (EGID). Her stomach gets inflamed with her own eosinophil cells. They would normally be marshaled to fight a parasite in her GI tract but in this case, there’s nothing to attack. So the cells make trouble on the lining of the stomach and cause pain and scarring. Right now, there’s no “magic bullet” to turn off these cells. My hope is some pharma scientists will come up with something to fill this unmet need.
In the waiting room before I saw my doctor at the cancer center in Seattle I overheard a woman on the phone speaking about her husband’s new diagnosis of pancreatic cancer. I was sitting at a patient education computer station nearby. When she was finished I introduced myself and showed her some webpages to give her education and hope: pancan.org and our Patient Power programs about the disease. She was grateful. I did tell her — and she already knew — that there was no miracle drug for pancreatic cancer and that it was a usually-fatal condition. But that there were exceptions and, hopefully, her husband would be one. Of course, wouldn’t an effective medicine be best? Read more »
*This blog post was originally published at Andrew's Blog*
November 3rd, 2010 by GarySchwitzer in Better Health Network, Health Policy, News, Opinion, Research
No Comments »

Continuing this week’s spontaneous theme (we didn’t make the claims and write the stories) of runaway enthusiasm for various screening tests by some researchers and journalists, HealthDay news service has reported on a study published in the Oct. 28 issue of the journal Nature that they say “provides new insight into the genetics of pancreatic cancer.” In the story, they let one of the researchers get away with saying, almost unchallenged:
“What’s important about this study is that it’s objective data in support of why everyone should be screened for pancreatic cancer.”
Mind you, this was a study that looked at tissue from just seven patients. The story continued with its breathless enthusiasm for the pancreatic cancer screening idea:
“In the future, new imaging techniques and blood tests will offer hope for early detection, the study noted. And just as people have a colonoscopy when they turn 50, “perhaps they should have an endoscopy of their upper gastrointestinal organs that includes an ultrasound of the pancreas,” said (the researcher).”
The very end of the story included some skepticism from Dr. Len Lichtenfeld of the American Cancer Society. Read more »
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
May 6th, 2010 by David H. Gorski, M.D., Ph.D. in Better Health Network, Health Policy, Opinion, Quackery Exposed, Research, True Stories
No Comments »

[Recently] I participated in a panel discussion at the Northeast Conference of Science and Skepticism (NECSS) with John Snyder, Kimball Atwood, and Steve Novella, who also reported on the conference. What I mentioned to some of the attendees is that I had managed to combine NECSS with a yearly ritual that I seldom miss, namely the yearly meeting of the American Association for Cancer Research (AACR) meeting.
There are two huge cancer meetings every year — AACR and the annual meeting of the American Society for Clinical Oncology (ASCO). AACR is the meeting dedicated to basic and translational research. ASCO, as the word “clinical” in its name implies, is devoted mainly to clinical research.
Personally, being a translational researcher myself and a surgeon, I tend to prefer the AACR meeting over ASCO, not because ASCO isn’t valuable, but mainly because ASCO tends to be devoted mostly to medical oncology and chemotherapy, which are not what I do as a surgeon. Each meeting draws between 10,000 to 15,000 or even more clinicians and researchers dedicated to the eradication of cancer. Read more »
*This blog post was originally published at Science-Based Medicine*
April 6th, 2010 by Jonathan Foulds, Ph.D. in Better Health Network, Expert Interviews, Health Policy, Health Tips, News, Opinion, Research, True Stories
2 Comments »

This week the respected CBS documentary news show “60 Minutes” included a feature on smokeless tobacco, focusing on the recent launch of snus in the United States. The show was relatively balanced in focusing on the main potential risks and benefits of snus.
It started by featuring a young man who enjoys using snus in places where he cannot smoke, while continuing with a pack-a-day smoking addiction. The interviewer gave him the bad news: “You are a dual user.”
It then had a segment with the widely respected Swedish nicotine addiction expert, Dr Karl Fagerstrom, who stated that snus is 90-99% less harmful than smoking (while admitting some risks, including of pancreatic cancer). Read more »
This post, Smokeless Tobacco And The U.S. Launch Of Snus, was originally published on
Healthine.com by Jonathan Foulds, Ph.D..
September 14th, 2009 by Dr. Val Jones in Announcements, Better Health Network, Expert Interviews, Health Policy, News, True Stories, Uncategorized
No Comments »
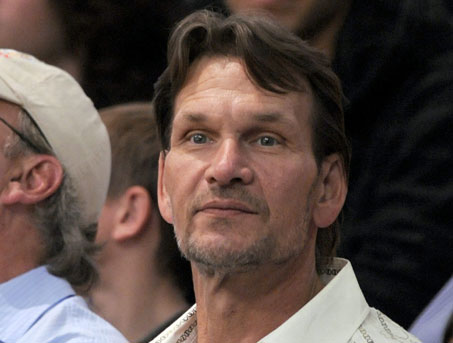
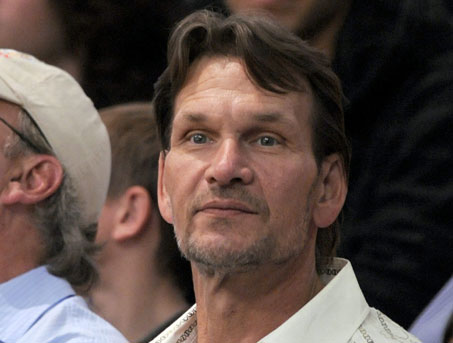 Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Pancreatic cancer is among the more deadly forms of cancer. I asked GI oncologist, Heinz-Josef Lenz, M.D., professor of medicine and professor of preventive medicine in the Division of Medical Oncology at the Keck School of Medicine at the University of Southern California, to explain why that’s so.
Dr. Val: Why is pancreatic cancer so much more deadly (i.e. less treatable) than many other forms of cancer?
Dr. Lenz: Unfortunately we don’t have very effective drugs for pancreatic cancer, which makes it one of the deadliest cancers of all. The median survival is about 8 months with metastatic disease. Even when the tumor is successfully removed there is a very high risk for tumor recurrence. We need more funding to better understand the risk for pancreatic cancer and identify and develop more effective therapies.
Dr. Val: Can you describe the typical course of metastatic pancreatic cancer?
Dr. Lenz: Unfortunately, the 5 year survival rate for pancreatic cancer is only 15 to 20%. The average survival after diagnosis is 12 to 19 months. The best predictor of long term survival is if the tumor is found and removed before it reaches 3 cm in size. Patients with metastatic pancreatic cancer are usually treated with a combination chemotherapy consisting of gemcitabine, tarceva, xeloda or oxaliplatin. However the response rates are (despite using aggressive combination therapies) low. Large clinical trials recently did not show any benefit from erbitux or avastin, again demonstrating that pancreatic cancer therapy is a difficult clinical challenge.
Dr. Val: Are certain populations at higher risk than others for pancreatic cancer?
Dr. Lenz: Age is the most important risk factor for this cancer. It is most common in individuals over age 50 and increases in frequency with age. Black men and women are slightly more likely to get pancreatic cancer (though the reasons for this are unclear), and men are slightly more likely than women to get the cancer. Other risk factors are smoking, diabetes, and obesity.
Dr. Val: If you suspect that someone is “high risk” for pancreatic cancer, what tests should he/she have?
Dr. Lenz: Patients with a genetic predisposition for breast cancer known as BRCA are also at higher risk for pancreatic cancer. There is also a familial form of pancreatic cancer. These high risk families are being followed up with specific screening plans. However there is not a reliable test for pancreatic cancer. Imaging with CT or MRI can miss pancreatic cancer and there is no reliable blood marker. The most common used is CA 19-9, which can be used for monitoring and diagnosis but is not elevated in all patients.
Dr. Val: What if the cancer is caught very early? Does that increase likelihood of survival?
Dr. Lenz: Absolutely. The best chance of survival is when the cancer is limited to the pancreas, and is surgically removed before it reaches a size of 3 centimeters. There are certainly people who have been cured this way, but unfortunately it’s very rare to catch the cancer at such an early stage since it usually has no symptoms until it’s quite advanced.
***
There is a wonderful advocacy group for those whose lives are touched by pancreatic cancer: PanCAN. One of PanCAN’s founders, Paula Kim, is a friend of mine and was inspired to create the organization after her dad was diagnosed with pancreatic cancer in 1999. At that time there was very little advocacy for this deadly disease. PanCAN helps people with pancreatic cancer find help and support.