November 30th, 2011 by StevenWilkinsMPH in Opinion
1 Comment »

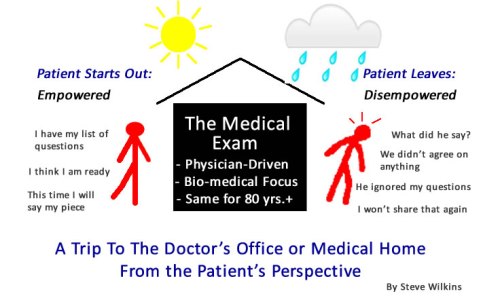
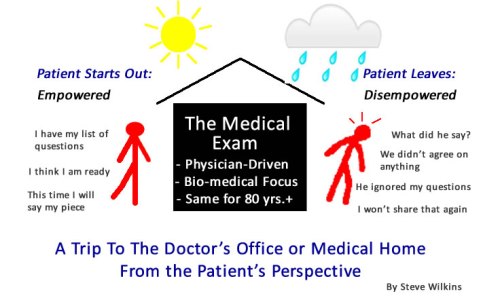
I may not know how to tell the difference between an empowered patient, an engaged patient, or an activated patient. But I do know that the fastest way to disempower, disengage, and de-activate any patient is a trip to the doctor’s office or the hospital. A visit to an average primary care physician (or specialist) is to an empowered/activated/engaged patient what Kryptonite is to Superman. It will stop all but the strongest willed patients dead in their tracks.
 We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
Things haven’t changed much in the 40 years since I was a kid sitting in Dr. Adam’s office. Read more »
*This blog post was originally published at Mind The Gap*
June 13th, 2011 by admin in Health Tips
No Comments »


In today’s fast-paced world, waiting — whether it’s at the doctor’s office, in line at the grocery store or for an Internet connection — is rarely considered a good thing.
But when it comes to certain medical conditions, delaying treatment while regularly monitoring the progress of disease — a strategy doctors refer to as “watchful waiting,” active surveillance or expectant management — may benefit some patients more than a rush to pharmaceutical or surgical options.
Patients want to know what they’re waiting for, says urologic oncologist E. David Crawford, MD, chairman of the Prostate Conditions Education Council and associate director of the University of Colorado Comprehensive Cancer Center.
The purpose is to watch in order to see whether a condition progresses. That way, patients and physicians know what kind of threat a disorder poses and they can make a better decision about how urgently treatment is needed. Some people might never need treatment, for instance with a slow-growing cancer. Other people can delay treatment for months or years.
Precancerous conditions may also be monitored with active surveillance. One example is Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
February 15th, 2011 by DavidHarlow in Health Policy, Research
No Comments »

There’s a growing recognition within the medical-industrial complex that the patient is a key element of the enterprise, and that patient satisfaction, patient experience, patient engagement, patient activation, and patient-centeredness are very important. Some research shows that patient activation yields better patient outcomes, and that patient activation can be measured.
Patient-centeredness and patient engagement are two of the key metrics to be used by the feds in describing Accountable Care Organizations (ACOs), if the internecine battles within government are resolved soon enough to actually release draft ACO regulations in time to allow for sufficient advance planning for the January 2012 go-live date. (Wearing one of my many hats, I’ve had the opportunity to submit a response to CMS regarding the RFI on these metrics on behalf of the Society for Participatory Medicine.) These measures go into the “meaningful use” hopper as well, as meaningful use stage 2 metrics are being reviewed.
In recent years, the federales have been measuring patient experience using the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys, and — coming soon to a bank account near you — there will be Medicare dollars tied to the scores on these questionnaires, not just dollars tied to the act of reporting scores.
As this emphasis on patient experience is unfolding, the Leapfrog Group is adding its voice to the chorus. I spoke this week with CEO Leah Binder and hospital survey director Matt Austin about the new patient experience measures they are adding to their 2011 hospital survey. In keeping with past practice, they will be asking hospitals to report three CAHPS measures (rather than asking folks to collect and report new measures). The three were selected as being representative of a hospital’s broader performance with respect to patient experience, and also because hospital performance on these measures is all over the map. Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
 We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…













