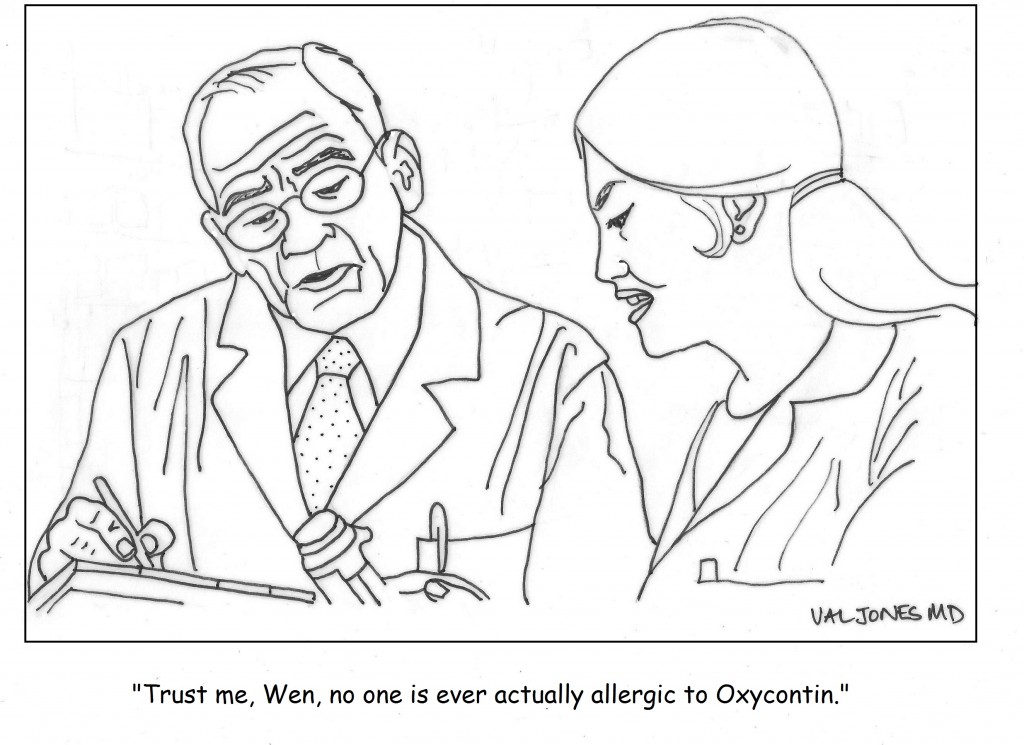
Cartoon: America’s Problem With Pain Meds

 Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.
Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.
Because EPIC keeps lists of home meds, discontinued meds, and current meds available for review and reactivation, it takes little more than one misplaced check box to order the wrong dose or type of medication. Physicians who transfer a patient to another service can indicate their intended medication list and keep it “on hold” for the receiving physician to review and approve. Unfortunately, the software’s tab system is so complex that it’s extremely difficult to find that list and activate it. Lost in a sea of admissions tasks and order boxes in different fonts, colors, and drop down menus, one often accidentally reviews and approves discontinued types and doses of medicines. The only protection against such errors is the hospital pharmacist.
With each new admission to the inpatient rehabilitation unit, I had to resort to calling a pharmacist for help. I was terrified that I would accidentally insert medication errors into the patient’s order set by carrying forward discontinued meds. The long-suffering pharmacists explained to me that “most physicians make medication order errors in EPIC with each admission.” They said that they regularly had to talk physicians out of throwing their computer out the window in a state of extreme frustration. They also said that their EPIC user environment looked very different (and less confusing) than what the physicians used, so that they couldn’t even provide real-time phone guidance regarding order entry process.
The scary thing is that EPIC has the largest market share of any EMR in the United States. It is also (in my experience) the most prone to medical errors due to its overly complex medication reconciliation process. I have used other EMRs that have far simpler and more intelligent medication order entry processes. Soarian (Sieman’s EMR, just sold to Cerner) has, for example, an outstanding order entry system. So my complaint is not that “all EMRs are bad” – it’s that some have particularly flawed designs that are causing real harm to untold millions of patients. We just haven’t documented the harm yet. I tremble at the thought of what we’d find.
Until electronic medication reconciliation is made safer, pharmacists will be working overtime to correct records and protect patients from carry over errors. I thank my lucky stars that I have had vigilant, determined pharmacists by my side as I cared for very complex, sick patients who were exceptionally vulnerable to dosing errors. There has never been a more important time to exercise caution when entering hospital medication orders, or to express your appreciation for pharmacists. Without their help we might all be experiencing medication errors of EPIC proportions.
 A nurse recently asked a very important question that bears repeating: What effect does long-term use of pain pills have on pregnant women? She was concerned because of the increase in number of pregnant women who are taking pain pills on a long term basis based on previous surgeries, accidents or a history of chronic pain.
A nurse recently asked a very important question that bears repeating: What effect does long-term use of pain pills have on pregnant women? She was concerned because of the increase in number of pregnant women who are taking pain pills on a long term basis based on previous surgeries, accidents or a history of chronic pain.
The most common “pain pills” prescribed are opiates which effectively eliminate or reduce pain but have a great tendency to be abused. Opioids are natural and synthetic type drugs that have the characteristics of morphine. It can only be obtained with a prescription and unfortunately physicians contribute to the problem of dependency and abuse through their lack of scrutiny regarding patient requests. My present home state of Florida has the unsavory distinction of being known as the country’s largest pill mill and it was reported that 80 percent of opiates were not dispensed by pharmacists but by physicians who dispense them from their offices. Consequently, the Florida legislators now prohibit physicians from dispensing opiates in their offices with rare exceptions.
Why are opiates or pain killers dangerous for pregnant women? Read more »
*This blog post was originally published at Dr. Linda Burke-Galloway*
 I sat in a dingy pharmacy near the Seattle airport over the holidays, waiting for an emergency prescription. For over two hours I watched a slow-moving line of people sign a book, pay and receive their prescription(s). The cashier told each customer picking up more than one prescription or a child’s prescription to wait on the side. In minutes, the harried white-haired pharmacist came over to ask the person if they were familiar with these medications, described how to take them, identified the side effects to look out for and demonstrated the size of a teaspoon for pediatric medications. Then he asked the person to repeat back – often in broken, heavily accented English – what he or she had heard and patiently went over the parts they didn’t understand.
I sat in a dingy pharmacy near the Seattle airport over the holidays, waiting for an emergency prescription. For over two hours I watched a slow-moving line of people sign a book, pay and receive their prescription(s). The cashier told each customer picking up more than one prescription or a child’s prescription to wait on the side. In minutes, the harried white-haired pharmacist came over to ask the person if they were familiar with these medications, described how to take them, identified the side effects to look out for and demonstrated the size of a teaspoon for pediatric medications. Then he asked the person to repeat back – often in broken, heavily accented English – what he or she had heard and patiently went over the parts they didn’t understand.
I was impressed. This is what every pharmacy should be like – except, of course, for the dinginess, the creeping line and the fact that it was so crowded I could overhear these conversations. Maybe if we got federal legislation enacted requiring pharmacists to offer counseling with each prescription filled, this kind of attention would be the norm, adherence to medication regimens would improve and drug-related injuries would be reduced.
Wait a minute. Someone already had that good idea. It was Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
New primary care arrangements show how primary care is evolving — or splitting apart, depending upon one’s perspective.
Retainer fees let one practice handle more patients by phone or email. But, points out Richard Baron, FACP, affluent communities can take advantage of such arrangements, and not every community is. And Sam Fink, FACP, of southern California says tele-visits are no substitute for hands-on care. In another model, nurse-led facilities service the poor in north Philadelphia, and more states are expanding the power of the pen to cover shortages.
Another trend is the shared medical appointment. Led by physicians and conducted by “behaviorists,” the sessions cover a half-dozen or more patients at a time for both primary and specialty care.
Even pharmacists are getting in on primary care. Blue Shield of California is trying a pilot project of pharmacists, believing they have the clinical and patient communication skills to be as effective as doctors, but for less cost. But primary care doctors aren’t completely ceding their profession. There are also pilot projects in California to train more doctors and steer them into communities facing a shortage of primary care services. (USA Today, Fox News, ACP Internist, New York Times, Whittier Daily News)
*This blog post was originally published at ACP Internist*
It’s no secret that doctors are disappointed with the way that the U.S. healthcare system is evolving. Most feel helpless about improving their work conditions or solving technical problems in patient care. Fortunately one young medical student was undeterred by the mountain of disappointment carried by his senior clinician mentors…
I am proud to be a part of the American Resident Project an initiative that promotes the writing of medical students residents and new physicians as they explore ideas for transforming American health care delivery. I recently had the opportunity to interview three of the writing fellows about how to…
Book Review: Is Empathy Learned By Faking It Till It’s Real?

I m often asked to do book reviews on my blog and I rarely agree to them. This is because it takes me a long time to read a book and then if I don t enjoy it I figure the author would rather me remain silent than publish my…
The Spirit Of The Place: Samuel Shem’s New Book May Depress You

When I was in medical school I read Samuel Shem s House Of God as a right of passage. At the time I found it to be a cynical yet eerily accurate portrayal of the underbelly of academic medicine. I gained comfort from its gallows humor and it made me…
Eat To Save Your Life: Another Half-True Diet Book

I am hesitant to review diet books because they are so often a tangled mess of fact and fiction. Teasing out their truth from falsehood is about as exhausting as delousing a long-haired elementary school student. However after being approached by the authors’ PR agency with the promise of a…