January 26th, 2015 by Dr. Val Jones in Health Policy, Opinion
53 Comments »
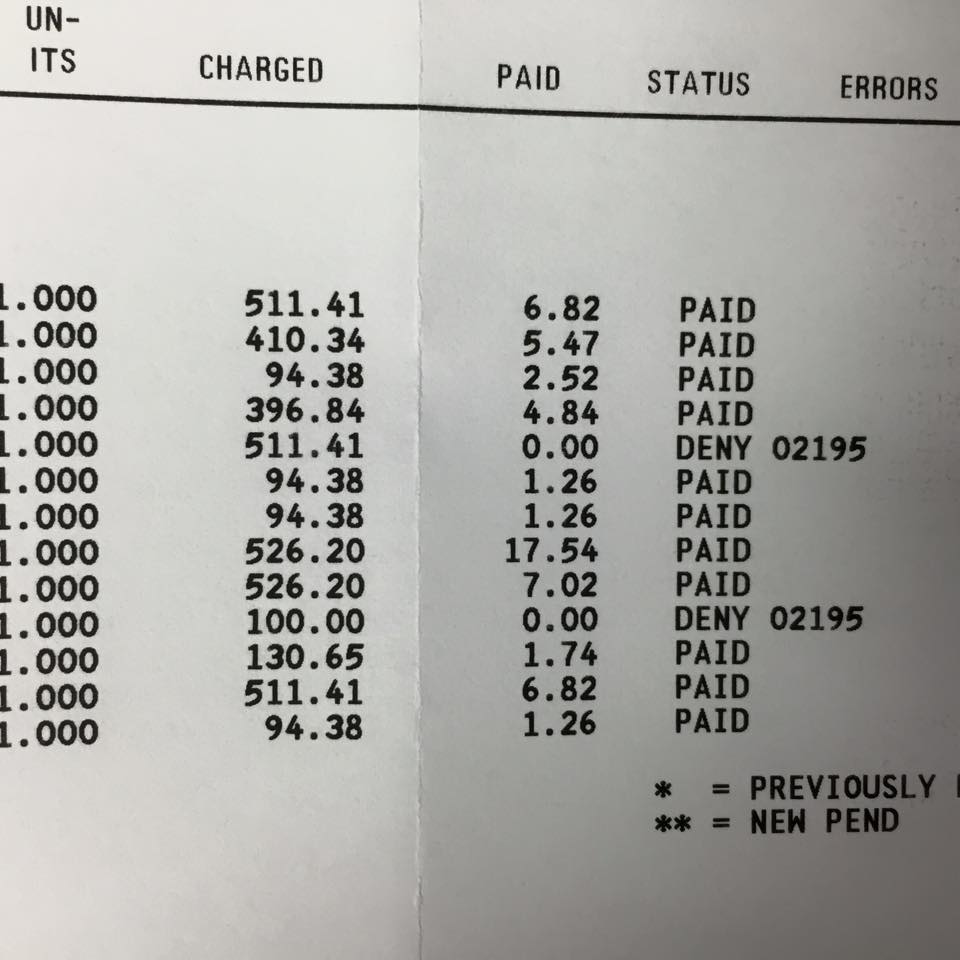 A physician friend of mine posted a copy of her Medicaid reimbursement on Facebook. Take a look at the charges compared to the actual reimbursement. She is paid between $6.82 and $17.54 for an hour of her time (i.e. on average, she makes less than minimum wage when treating a patient on Medicaid).
A physician friend of mine posted a copy of her Medicaid reimbursement on Facebook. Take a look at the charges compared to the actual reimbursement. She is paid between $6.82 and $17.54 for an hour of her time (i.e. on average, she makes less than minimum wage when treating a patient on Medicaid).
The enthusiasm about expanding Medicaid coverage to the previously uninsured seems misplaced. Improved “access” to the healthcare system via Medicaid programs surely cannot result in lasting coverage. In-network physicians will continue to dwindle as their office overhead exceeds meager reimbursement levels.
In reality, treating Medicaid patients is charity work. The fact that any physicians accept Medicaid is a testament to their generosity of spirit and missionary mindset. Expanding their pro bono workloads is nothing to cheer about. The Affordable Care Act’s “signature accomplishment” is tragically flawed – because offering health insurance to people that physicians cannot afford to accept is not better than being uninsured.
After all, improved access to nothing… offers nothing. Inviting physicians to work for less than minimum wage so that politicians can crow about millions of uninsured Americans now having access to healthcare, is ridiculous. Medicaid expansion is widening the gap between the haves and the have-nots. The saddest part is that the have-nots just don’t realize it yet.
January 29th, 2011 by KevinMD in Health Policy, Opinion
No Comments »

I recently pointed to a BMJ study concluding that pay for performance doesn’t seem to motivate doctors. It has been picking up steam in major media with TIME, for instance, saying: “Money isn’t everything, even to doctors.”
So much is riding on the concept of pay for performance, that it’s hard to fathom what other options there are should it fail. And there’s mounting evidence that it will.
Dr. Aaron Carroll, a pediatrician at the University of Indiana, and regular contributor to KevinMD.com, ponders the options. First he comments on why the performance incentives in the NHS failed:
Perhaps the doctors were already improving without the program. If that’s the case, though, then you don’t need economic incentives. It’s possible the incentives were too low. But I don’t think many will propose more than a 25 percent bonus. It’s also possible that the benchmarks which define success were too low and therefore didn’t improve outcomes. There’s no scientific reason to think that the recommendations weren’t appropriate, however. More likely, it’s what I’ve said before. Changing physician behavior is hard.
So if money can’t motivate doctors, what’s next? Physicians aren’t going to like what Dr. Carroll has to say. Read more »
*This blog post was originally published at KevinMD.com*
December 17th, 2010 by GarySchwitzer in Health Policy, News
No Comments »

I’ve been traveling in Europe, including giving a talk at the Salzburg Global Seminar on involving and informing patients in healthcare decisions. In that presentation, I talked about promotion of a newer form of cancer radiation therapy called intensity-modulated radiation therapy (IMRT).
So I want to point out that while I’ve been away the Wall Street Journal published an important piece on this very topic under the headline “A Device to Kill Cancer, Lift Revenue.” An excerpt:
Roughly one in three Medicare beneficiaries diagnosed with prostate cancer today gets a sophisticated form of radiation therapy called IMRT. Eight years ago, virtually no patients received the treatment.
The story behind the sharp rise in the use of IMRT—which stands for intensity-modulated radiation therapy—is about more than just the rapid adoption of a new medical technology. It’s also about financial incentives.
Taking advantage of an exemption in a federal law governing patient referrals, groups of urologists across the country have teamed up with radiation oncologists to capture the lucrative reimbursements IMRT commands from Medicare.
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
November 9th, 2010 by GarySchwitzer in Better Health Network, Health Policy, News, Opinion
No Comments »

Take medical uncertainty. Add financial incentive to treat. Voila! Increased utilization. Now take away financial incentive to treat. Guess what you get?
MedPageToday explains, in the case of hormone therapy for prostate cancer:
Medicare accomplished what clinical guidelines and evidence-based medicine couldn’t: it reduced unnecessary use of androgen deprivation therapy (ADT) in prostate cancer.
Inappropriate use decreased by almost 30% from 2003 to 2005, following enactment of the Medicare Modernization Act, which lowered physician reimbursement for ADT. Appropriate use of ADT did not change during the same time period, according to an article in the Nov. 4 issue of the New England Journal of Medicine.
“Our findings suggest that reductions in reimbursement may influence the delivery of care in a potentially beneficial way, with even the modest [reimbursement] changes in 2004 associated with a substantial decrease in the use of inappropriate therapy,” Vahakn B. Shahinian, MD, of the University of Michigan in Ann Arbor, and co-authors wrote in conclusion.
“The corollary is that reimbursement policies should be carefully considered to avoid providing incentives for care for which no clear benefit has been established. The extreme profitability of the use of gonadotropin-releasing hormone (GnRH) agonists during the 1990s probably contributed to the rapid growth in the use of ADT for indications that were not evidence-based.”
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
August 9th, 2010 by Edwin Leap, M.D. in Better Health Network, Health Policy, Opinion, True Stories
No Comments »

This is my column in [the August 3rd] Atlanta Journal Constitution:
Secretary of Labor Hilda Solis recently produced an interesting public service announcement. In it, she stated that every worker deserves to be paid fairly for his or her labor (whether the worker is documented or not), and offered both a website and telephone hot-line which workers could use to report unfair payment by employers. (Incidentally, here’s the link: www.dol.gov/wecanhelp.) In the video, she stated succinctly, “You work hard, and you deserve to be paid fairly.”
Those of us who practice medicine completely agree. So we might reasonably ask if this announcement also applies to physicians who are undercompensated for their work. This routinely happens when patients are covered by Medicare and Medicaid, or by large insurance companies like Blue Cross/Blue Shield, which routinely negotiate unfair physician fees using their collective weight in bargaining. (Even as their executives bring home tidy bonuses that are clearly padded by denials). Read more »
*This blog post was originally published at edwinleap.com*
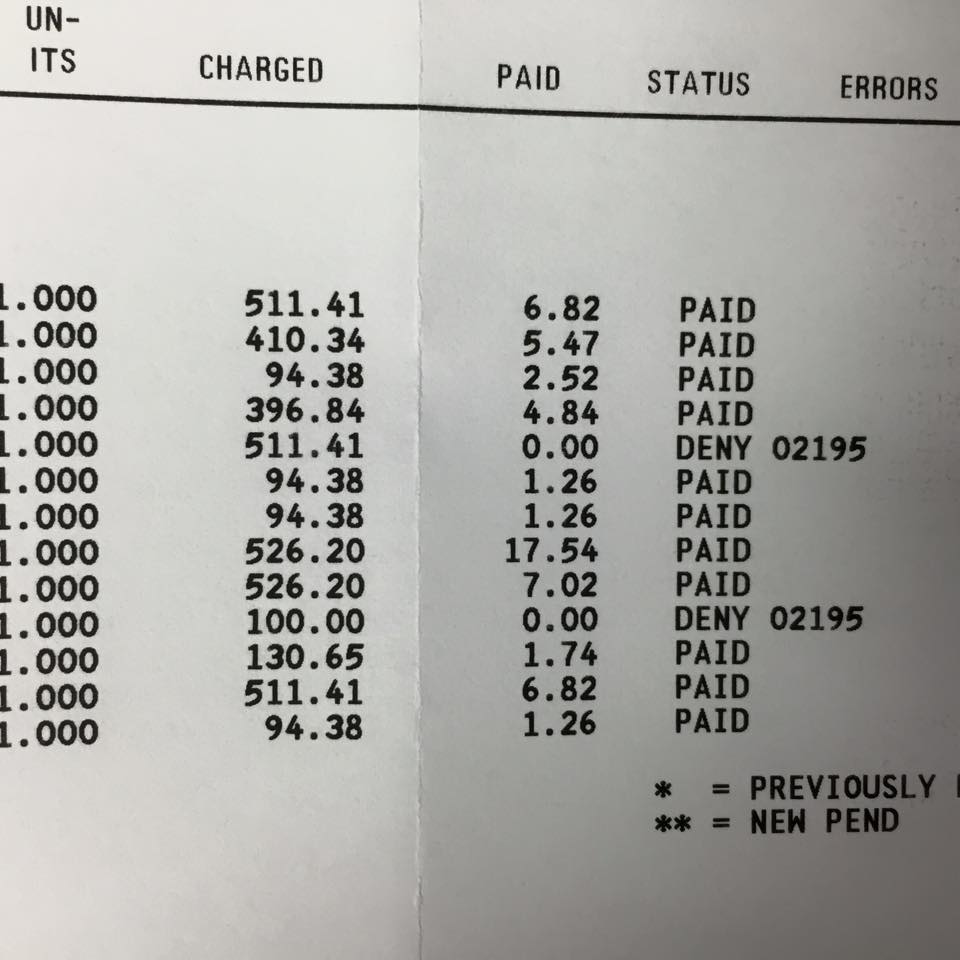 A physician friend of mine posted a copy of her Medicaid reimbursement on Facebook. Take a look at the charges compared to the actual reimbursement. She is paid between $6.82 and $17.54 for an hour of her time (i.e. on average, she makes less than minimum wage when treating a patient on Medicaid).
A physician friend of mine posted a copy of her Medicaid reimbursement on Facebook. Take a look at the charges compared to the actual reimbursement. She is paid between $6.82 and $17.54 for an hour of her time (i.e. on average, she makes less than minimum wage when treating a patient on Medicaid).












