January 4th, 2009 by Dr. Val Jones in Opinion
2 Comments »
I was a little surprised by a recent reader comment suggesting that pharmaceutical companies are no different than tobacco manufacturers. While I am strongly opposed to misleading pharmaceutical marketing tactics, the bottom line is that most drugs have a legitimate therapeutic value. Tobacco, on the other hand, is a known carcinogen with no medical value that I can think of. This comparison, however, brought into focus a common underlying assumption: that for-profit companies are inherently less ethical than non-profit and academic centers.
I’d like to question the tendency to absolve academic centers of any possible wrongdoing on the basis of their educational reputation or non-profit status. Of course, financial gain is not the only motivator behind endeavors, initiatives, and behaviors – though it may be the easiest to measure.
As a medical student I witnessed a sad example of academic misbehavior. Senior residents in the department of plastic surgery were performing liposuction procedures after hours for cash. When a patient experienced an infectious complication from a thigh liposuction procedure, an investigation ensued. The residents claimed to be putting the cash into the residency fund, to be used to support travel, lodging and participation in annual assemblies – therefore exonerating themselves of wrong-doing.
It is unclear if the department chair was fully aware of what the residents were up to, though he was reprimanded, terminated, and ended up teaching at another institution. The plastic surgery department lost its accreditation, and all of the residents had to finish their training elsewhere. As for me, I lost my mentor (the department chair) and ended up not pursuing a career in surgery. There certainly was a lot of fall out from that debacle on all sides.
A case of academic double standards was highlighted recently by Dr. George Lundberg in a Medscape editorial where journal editors claimed that continuing medical education (CME) courses should never be sponsored by for-profit companies. Meanwhile the journal accepted advertising from these same companies:
…The JAMA editors who wrote in 2008: “…providers of continuing medical education courses should not condone or tolerate for-profit companies…providing funding or sponsorship for medical education programs….” This is from a publication that, for more than 100 years, has been supported primarily by advertising revenue, mostly pharmaceutical. The editors will say “yes, but we follow rules to prevent bias or improper influence.” True. So do we, a for-profit company, follow rules that prevent bias and improper influence.
On the positive side, there are many examples of for-profit companies who cultivate a culture of environmental responsibility and charity – Ben & Jerry’s, SC Johnson, and Patagonia come to mind. And let’s not forget the foundations created by Bill and Melinda Gates, Warren Buffet and many others thanks to overflow from for-profit endeavors.
In the end, conflicts of interest, hidden agendas, and secret quid pro quos are a matter of individual character and corporate culture. The people who build a company (or a country) have more to do with its behaviors and processes than the simple label “for profit” or “non profit” or any assumptions made at such a superficial level.
We are all biased in many ways, both consciously and unconsciously. The best we can do is to strive for transparency. It may be best to judge each entity and/or individual by their degree of transparency rather than profit status, academic status, or subject matter expertise. For-profit companies can be highly ethical, and academic centers can be rife with undisclosed conflicts and questionable behaviors.
Healthcare organizations should not avoid or incur scrutiny based on their profit status alone. Bias comes in many forms – and the best we can do is work for the good of others in full knowledge of the influences around us.
December 22nd, 2008 by Dr. Val Jones in Medblogger Shout Outs
No Comments »
Here’s my weekly round up of quotable quotes from my peers:
NHS Blog Doctor: Antibiotics do not cure snot. [Please go to the site for a fabulous illustrative photo.]
KevinMD: Since work-hours were restricted in 2003, there are no studies that have shown any marked improvements in patient safety or outcomes. Worse, errors have arisen from the so-called “patient hand-off,” the period of communication where rested doctors replaces those who are fatigued. Does increasing the frequency of patient hand-offs outweigh the benefit of better rested doctors?
Richard Reece, MD: The moral for doctors: Don’t expect as much leverage as in the past when negotiating with hospitals, even though you represent their main revenue stream.
Paul Levy: The medical community in Boston likes to boast about the medical care here, but we don’t do a very good job holding ourselves accountable.
Dr. Wes: Thanks to exorbitant costs of implementing EMRs in physician practices, the Medicare requirements for billing and prescribing electronically, and the prohibitive documentation requirements mandated by CMS in the name of “quality,” independent physician practices of all types will have no choice but capitulate to larger entities that have a fully integrated electronic medical record paired with collection software.
Heart found in a car wash (h/t Dr. Wes)
Ramona Bates, MD: I don’t think I would ever want to be part of doing a posthumous face lift or blepharoplasty or other cosmetic procedure, but I would be willing to debulk tumors if it would help families or individuals say “goodbye” more easily.
WhiteCoat Rants: For $79 you can blow into your iPod and it will play you a song if your blood alcohol is more than 0.08. You know this device wasn’t made for parents.
Just what we need. A bunch of drunk teenagers farting around with their iPods and getting into a “who can get the highest blood alcohol” contest.
The Happy Hospitalist: It frightens me to hear people say they want to work in medicine and work in a similar capacity as physicians, evaluating, diagnosing and managing disease, but not want to put in the time and sacrifice to be residency trained in depth and scope…
Science-Based Medicine: Our soldiers, grievously wounded in combat, deserve only the best science-based therapy available… If I were to propose treating our injured soldiers with bloodletting and toxic metals (both common methods in the 1700s and early 1800s) based on the concept that it would put the “imbalance of the four humors” back into balance, the Pentagon and the military medical establishment would toss me out on my ear as a dangerous quack–and rightly so. But introduce a method that claims “ancient Chinese wisdom” based on somehow magically redirecting the flow of a mysterious “life energy” by sticking small needles into parts of the body that correspond to no known anatomic structures through which “qi” flows, and suddenly the Air Force is funding a program to train medics and physicians treating our wounded soldiers how to do this method based on the same amount of convincing scientific evidence that qi exists as for the four humors (none) and in the face of no strong clinical evidence that it’s any better than a placebo.
Rural Doctoring: Hospitalists, take note: this is an example of why people go ape-sh*t crazy in the hospital:
• Her right arm is completely immobilized to protect the graft site.
• Her left arm has a heplocked IV in it.
• Half her head is shaved because the surgeon took the donor skin from the scalp.
• She’s vegetarian and the cafeteria sent her chicken for lunch.
• Dinner was vegetarian but she can’t really cut up a baked potato with only one hand.
• The hospital has double rooms and is running at capacity, so the staff is harried.
• Her roommate is an elderly, demented woman who keeps trying to get out of bed by herself and objects to the TV being on. So far, all she’s said to us is “Mind your own business!”
October 19th, 2008 by Dr. Val Jones in Expert Interviews
No Comments »

Even though I live in DC it was my first visit to the Department of State. I was surprised by the level of security (I passed through 2 metal detectors to get to the conference) and the multitude of languages spoken by the attendees. Many were wearing headphones, which were connected to a translator service. The lectures were rapidly translated into the various languages of the audience members (the way it would for the United Nations meetings), though I enjoyed the ability to listen directly to the speakers in my native tongue.
I was able to interview a keynote speaker, Joe Harford, Ph.D., the Director of the Office of International Affairs, of the National Cancer Institute. Here’s what he had to say:
Dr. Val: Why is the risk of breast cancer (in the US) greater now than in previous generations?
Dr. Harford: The main cause of the increase is related to changes in reproductive patterns within the population as a whole. Women who have fewer children (and later in life) tend to have higher risk of breast cancer. This is associated with hormones – the breast is a hormonally responsive organ and breast cells that convert to tumor cells also have hormone receptivity. Pregnancy and breast feeding are protective for breast tissue. Women can check out their risk for developing breast cancer by filling out this
short, online assessment tool at the NCI.
Read more »
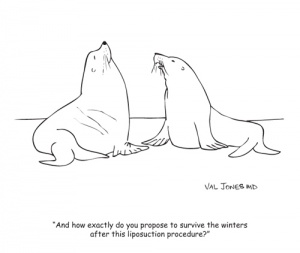
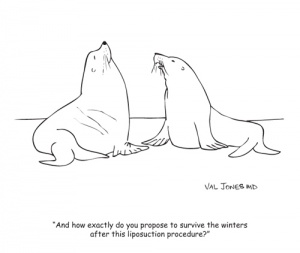
October 17th, 2008 by Dr. Val Jones in Friday Funny
5 Comments »
I’m introducing a new feature to the blog: a weekly cartoon posted every Friday. If you’d like to subscribe to the cartoon feed (perhaps you’d like to feature the weekly cartoon on your website?) please contact john.crotty@getbetterhealth.com
Enjoy your weekly dose of humor from Dr. Val! By the way, what time on Friday should I publish these do you think? I’d appreciate your feedback.
October 7th, 2008 by Dr. Val Jones in Medblogger Shout Outs
No Comments »
While I was “homeless” my blogging friends kindly invited me to guest post at their websites. Ramona Bates at Suture For A Living posted this for me:
I have a great plastic surgeon friend who offered to fill a facial scar for me. I was bitten in the face by a dog when I was very young, and the small (1/2 inch) divot of flesh from my cheek still bothers me slightly. I’ve generally ignored it but thought it might be fun to see if it could be corrected in any way – so I happily agreed to try a Restylane (hyaluronic acid) injection.
My surgeon and I decided not to use any numbing medication because it distorts the contours of the face, making correction more challenging. So I tried my best not to squirm as he inserted a fairly long needle parallel to my nose…
To read the rest of the post, please click here.