September 5th, 2014 by Dr. Val Jones in Health Policy, Opinion
1 Comment »
 As a physician who openly despises many aspects of current EMRs (see “How An EMR Gave My Patient Syphilis” or “The Medical Chart: Ground Zero For The Deterioration Of Patient Care” ) I recognize that they are here to stay. And so, since we’re all stuck with these digital middlemen, I have some suggestions (based on popular social media platform functionality) for making them better.
As a physician who openly despises many aspects of current EMRs (see “How An EMR Gave My Patient Syphilis” or “The Medical Chart: Ground Zero For The Deterioration Of Patient Care” ) I recognize that they are here to stay. And so, since we’re all stuck with these digital middlemen, I have some suggestions (based on popular social media platform functionality) for making them better.
1. Likes. Healthcare providers should be able to “vote up” an excellent note in the medical record. Let’s face it, not all doctors are equally good at documentation. Untold hours of our time are spent trying to cull through pages of auto-populated, drop-down-box checks to figure out what’s actually going on with a patient on a particular day. Once in a while you stumble upon some comprehensive free text that a physician took the time to type after a previous encounter, and suddenly everything becomes clear. If there were a way to flag or “like” such documents, it would help other readers orient themselves more quickly to a patient’s history. A “liking” system is desperately needed in EMRs and would be a valuable time saver, as well as encouragement to physicians who document notes well. Hospitals could reward their best note makers with public recognition or small monetary bonuses.
2. #Hashtags. Tagging systems are sorely lacking in medical records systems, which makes them very difficult to search. Patients make multiple visits for various complaints, often with numerous providers involved. If physicians had the ability to review notes/records unique to the complaint that they are addressing, it would save a lot of time. Notes could be tagged with keywords selected by the author and permanently recorded in the EMR. This would substantially improve future search efforts. Even if the EMR generated 10 search terms (based on the note) and then asked the physician to choose the 3 most relevant to the current encounter, that would be a step in the right direction.
3. Selfies. Medical records would benefit from patient-identifier photographs. In a busy day where 20-30 patients are treated and EMR notes are updated after the patients have gone home, a small patient photograph that appears on each documentation page will serve the physician well in keeping details straight. Patients should be able to upload their favorite portrait to the EMR if the standard one (perhaps taken during the intake process) is not acceptable to them. In my experience, nothing brings back physical exam and history details better than a photograph of the patient.
4. Contextual links. All EMRs should provide links to the latest medical literature (on subjects specifically related to the patient’s current diseases and conditions) in a module on the progress note page. UpToDate.com and other reference guides could easily supply the right content (perhaps based on diagnosis codes). This will help physicians practice evidence-based medicine and keep current with changes in recommended treatment practices.
5. Microblogging. Sometimes there are important “notes to self” that a physician would like to make but don’t need to be part of the official medical record. EMRs should provide a free-text module (like a digital sticky note) for such purposes. These sticky notes should not be admissible in court as part of the medical record, and should not be uploaded to the cloud. Content included in these notes could include social information (patient’s daughter just had a healthy baby girl), hunches (patient looks slightly pale today – will check H&H next time if no change), and preliminary information (remember to review radiology result before calling patient next Tues).
It is my hope that EMRs will slowly adopt some best practices from top social media platforms. After all, if millions of users are effectively using voting, tagging, linking, searching and imaging in their daily online lives, it only makes sense to capitalize on these behaviors within the constraints of the medical environment. Maintaining strict confidentiality and appropriate professional boundaries (often missing in the social media world at large) is certainly possible with EMRs. Let’s build a better information capture and retrieval process for the sake of our patients, and our sanity.
***
At least one EMR is already providing #3 and #5 as part of its software: see MDHQ.com Are you aware of any others already implementing these ideas?
May 29th, 2014 by Dr. Val Jones in Health Policy, Opinion
4 Comments »
 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In a policy environment where quality measures and patient satisfaction ratings are becoming the basis for reimbursement rates, one wonders how VMS software is getting traction. Perhaps desperate times call for desperate measures, and the challenge of filling employment gaps is driving interest in impersonal digital match services? Rural hospitals are desperate to recruit quality candidates, and with a severe physician shortage looming, warm bodies are becoming an acceptable solution to staffing needs.
As distasteful as the thought of computer-matching physicians to hospitals may be, the real problems of VMS systems only become apparent with experience. After discussing user experience with several hospital system employees and reading various blogs and online debates here’s what I discovered:
1. Garbage In, Garbage Out. The people who input physician data (including their certifications, medical malpractice histories, and licensing data) have no incentive to insure accuracy of information. Head hunter agencies are paid when the physicians/nurses they enter into the database are matched to a hospital. To make sure that their providers get first dibs, they may leave out information, misrepresent availability, and in extreme cases, even falsify certification statuses. These errors are often caught during the hospital credentialing process, which results in many hours of wasted time on the part of internal credentialing personnel, and delays in filling the position. In other cases, the errors are not caught during credentialing and legal problems ensue when impaired providers are hired accidentally.
2. Limitation of choice. The non-compete contracts associated with VMS systems typically prevent hospital physician recruiters from contacting staffing agencies directly to fill their needs. This forces the hospital to rely on the database for all staffing leads. At least 68% of staffing agencies do not participate with VMS systems, so a large portion of the most carefully vetted professionals remain outside the VMS, inaccessible to those who contracted to use it.
3. Extra hospital employee training required. There are hundreds of proprietary VMS systems in use. Each one requires specialized training to manage everything from durable medical equipment to short term surgical staff. In cases where hospital staff are spread too thin to master this training, some VMS companies are pleased to provide a “managed service provider” or MSP to outsource the entire recruitment process. This adds additional layers, further removing the hospital recruiter from the physician.
4. Providers hate VMS systems. As anyone who has read a recent nursing blog can attest, VMS systems are universally despised by the potential employees they represent. VMS paints professionals in black and white, without the ability to distinguish quality, personality, or perform careful reference checks. They force down salaries, may rule out candidates based on where they live (travel costs), and provide no opportunity to negotiate salary vis-a-vis work load. When a hospital opts to use a VMS system as a middle man between them and the staffing agencies, the agencies often pass along the cost to the providers by offering them a lower hourly rate.
5. Provider privacy may be compromised. Once a physician or nurse curriculum vitae (CV) is entered into the VMS database the agency recruiter who entered it has 1 year (I can’t confirm that this is true for all systems) to represent them exclusively. After that, the CV is often available for any recruiter who has access to that VMS to view or pitch to any client. There is a wide variety of agency quality in the healthcare staffing industry, with some being highly ethical and selective in choosing their clients (only quality hospitals) and providers (carefully screened). Others are transactional, bottom-feeders with all the scruples of a used car salesman. When your data is in a VMS, one minute you might be represented by a caring, thoughtful recruiter who understands and respects your career needs, and the next (without your informed consent) you’ll be matched to a bankrupt hospital undergoing investigation by the Department of Health by a gum-chewing salesman who threatens you with a lawsuit if you don’t complete an assignment for half the pay you usually receive.
6. No cost savings, only increased liability. In the end, some hospitals who have tried VMS systems say that their decreased hiring costs have not resulted in overall savings. While they may see a downward shift in salary paid to their temporary work force, they get what they pay for. Just one “bad hire” who causes a medical malpractice lawsuit can eat up salary savings for an entire year of VMS. Not to mention the increased costs associated with a slower hiring process, attrition from poor fits, and the inconvenience of having to re-recruit for positions over and over again. Providers also lose out on career opportunities while they’re “on hold” during a prolonged hiring process. And for those who layer on a MSP, they lose control of the most important hospital quality and safety line of defense – choosing your own doctors and nurses.
In summary, while the idea of using a software matching service for recruiting physicians and nurses to hospitals sounds appealing at first, the bottom line is that reducing care providers to a group of numerical fields removes all the critical nuance from the hiring process. VMS, with their burdensome non-competes, cumbersome technology, and lack of quality control are an unwelcome new middle man in the healthcare staffing environment. It is my hope that they will be squeezed out of the business based on their own inability to provide value to a healthcare system that craves and rewards quality and excellence in its staff.
Job matching requires thoughtful hospital recruiters in partnership with ethical, experienced agencies. Choosing one’s hospital gauze vendor should involve a different selection algorithm than hiring a new chief of surgery. It’s time for physician and nurse groups to take a stand against this VMS-inspired commoditization of medicine before its roots sink in too deeply and we all become mere line items on a hospital vendor list. So next time you doctors and nurses plan to work a temporary assignment, ask your recruiter if they use a VMS system. Avoiding those agencies who do may mean a much better (and higher paying) work experience.
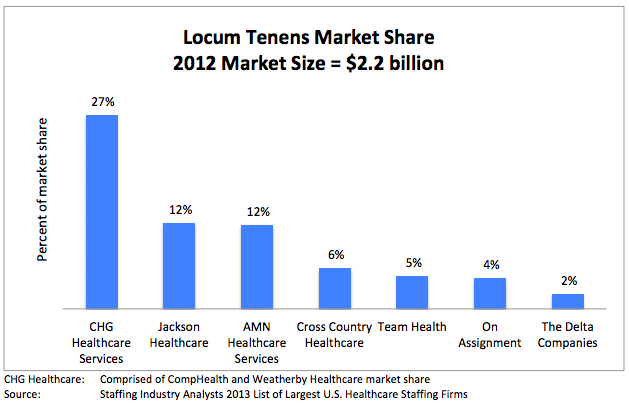
*Locum tenens (filling hospital staffing needs with part time or traveling physicians and nurses) is big business. Here is a run down of the estimated market size and its key industry leaders (provided by CompHealth):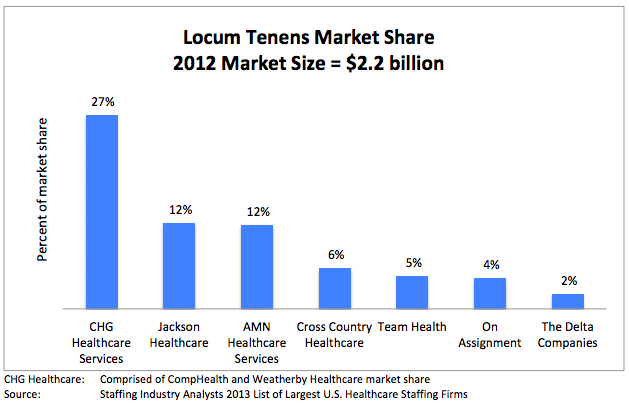
December 13th, 2011 by Dinah Miller, M.D. in Opinion
No Comments »

 In yesterday’s post on e-prescribing, the issue of patient confidentiality came up in the context of doctors being able to see a patient’s full medication history in an electronic program, and one commenter brought up that she doesn’t necessarily want to tell her shrink about a yeast infection, perhaps because she finds it embarrassing. The writer of the post, a guest blogger, suggested that this might lead to useful information that should be addressed in therapy, for example the patient’s sexual life.
In yesterday’s post on e-prescribing, the issue of patient confidentiality came up in the context of doctors being able to see a patient’s full medication history in an electronic program, and one commenter brought up that she doesn’t necessarily want to tell her shrink about a yeast infection, perhaps because she finds it embarrassing. The writer of the post, a guest blogger, suggested that this might lead to useful information that should be addressed in therapy, for example the patient’s sexual life.
Years ago, I remember being a bit taken back when a patient brought up some rather problematic (to him) sexual issues in his marriage. It wasn’t the nature of the issues that surprised me (I spent more than a decade consulting to a sexual behaviors unit and I spent several months of residency training on an inpatient sexual disorders unit: it takes a lot to shock me). What surprised me was that this was the first I was hearing about this issue after seeing the patient for 5 years of psychotherapy. He had a secret life.
There’s not really much to do about this. One can only Read more »
*This blog post was originally published at Shrink Rap*
October 28th, 2011 by DavidHarlow in Opinion
No Comments »
I’m back from my pilgrimage to Rochester, MN for the Third Annual Health Care Social Media Summit at the Mayo Clinic, presented by Ragan Communications. I had a great time, and want to share the experience with you. So please take a look at the archived #mayoragan tweets, my presentation on health care social media and the law, and my blog posts about the pre-conference and the summit itself posted at HealthWorks Collective. Here are some excerpts:
Mayo Ragan Social Media Summit Pre-Conference:
A recurring theme in my hallway conversations [today] was that it is impossible to transplant a successful program from one location to another without taking into account myriad local conditions (social media program, heart transplant program – same problem). As I always say to folks Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
October 10th, 2011 by DavidHarlow in Health Policy, News
No Comments »
On September 14, HHS released for comment draft lab results regulations that will, if finalized, effectively bathe the Achilles’ heel of health data in the River Styx of ¡data liberación! All lab results will be made available to patients, just like all other health data. (See the HHS presser and YouTube video from the recent consumer health summit. Todd Park, HHS CTO, is also the chief activist for what he calls ¡data liberación!)
Forgive me for mixing my metaphors (or whatever it is I just did), but even though there are just a couple dozen words of regulations at issue here, this is a big deal.
When HIPAA established a federal right for each individual to obtain a copy of his or her health records, in paper or electronic format, there were a couple of types of records called out as specifically exempt from this general rule of data liberation, in the HIPAA Privacy Rule, 45 CFR § 164.524(a)(1): psychotherapy notes, information compiled for use in an administrative or court proceeding, and lab results from what is known as a CLIA lab or a CLIA-exempt lab (including “reference labs,” as in your specimens get referred there by the lab that collects them, or freestanding labs that a patient may be referred to for a test; these are not the labs that are in-house at many doctors’ offices, hospitals and other health care facilities — the in-house labs are part of the “parent” provider organization and their results are part of the parents’ health records already subject to HIPAA).
(“CLIA” stands for the Clinical Laboratory Improvement Amendments of 1988, which established quality standards for certain laboratory testing.)
This carveout of lab results from patient-accessible records has long been a thorn in the side of the e-patient. This month, Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
 As a physician who openly despises many aspects of current EMRs (see “How An EMR Gave My Patient Syphilis” or “The Medical Chart: Ground Zero For The Deterioration Of Patient Care” ) I recognize that they are here to stay. And so, since we’re all stuck with these digital middlemen, I have some suggestions (based on popular social media platform functionality) for making them better.
As a physician who openly despises many aspects of current EMRs (see “How An EMR Gave My Patient Syphilis” or “The Medical Chart: Ground Zero For The Deterioration Of Patient Care” ) I recognize that they are here to stay. And so, since we’re all stuck with these digital middlemen, I have some suggestions (based on popular social media platform functionality) for making them better.

 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.