October 17th, 2014 by Dr. Val Jones in Opinion, True Stories
No Comments »
 Electronic medical records (EMRs) now play a part in the daily documentation routine for most physicians. While improvements in access to patient data, legibility of notes, and ease of order entry are welcome enhancements, there is a significant downside to EMRs as well. Although I’ve blogged about my frustrations with nonsensical, auto-populated notes and error carry-forward, there is a more insidious problem with reliance on EMRs: digital dependency.
Electronic medical records (EMRs) now play a part in the daily documentation routine for most physicians. While improvements in access to patient data, legibility of notes, and ease of order entry are welcome enhancements, there is a significant downside to EMRs as well. Although I’ve blogged about my frustrations with nonsensical, auto-populated notes and error carry-forward, there is a more insidious problem with reliance on EMRs: digital dependency.
The idea of digital dependency first occurred to me during a conversation with a young medical resident at a hospital where we share patients. I was bemoaning the fact that I was being forced to use hospital-designed templates for admission notes, rather than a dictation system or carefully crafted note of my own choosing. She looked at me, wide-eyed and said:
“You’ve worked without templates? How do you even know where to begin? Can you really dictate an entire note off the top of your head? I couldn’t live without templates.”
As I stared back at her with an equal amount of bewilderment, I slowly realized that her thinking had been honed for drop-down menus and check boxes. Over time, she had lost the ability to construct narratives, create a cohesive case for her diagnostic impressions, and justify her patient plan of action. To this bright, highly trained mind, clinical reasoning was an exercise in multiple choice selection. Her brain had been optimized for the demands of an EMR template, and mine was a relic of the pre-EMR era. I was witnessing a fundamental cognitive shift in the way that medicine was practiced.
The problem with “drop-down medicine” is that the advantages of the human mind are muted in favor of data entry. Physicians in this model essentially provide little benefit over a computer algorithm. Intuition, clinical experience, sensory input (the smell of pseudomonas, the sound of pulmonary edema, the pulsatile mass of an aneurysm) are largely untapped. We lose our need for team communication because “refer to my EMR note” is the way of the future. Verbal sign-outs are a thing of the past it seems, as those caring for the same patient rely on their digital documentation to serve in place of human interaction.
My advice to the next generation of physicians is to limit your dependency on digital data. Like alcohol, a little is harmless or possibly healthy, but a lot can ruin you. Leverage the convenience of the EMR but do not let it take over your brain or your patient relationships. Pay attention to what your senses tell you during your physical exam, take a careful history, listen to family members, discuss diagnostic conundrums with your peers, and always take the time for verbal sign outs. Otherwise, what advantage do you provide to patients over a computer algorithm?
Am I a curmudgeon who is bristling against forward progress, or do I have a reasonable point? Judging from the fact that my young peers copy and paste my assessment and plans into their progress notes with impressive regularity, I’d say that templatized medicine still can’t hold a candle to thoughtful prose. Even the digitally dependent know this. 🙂
May 29th, 2014 by Dr. Val Jones in Health Policy, Opinion
4 Comments »
 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In a policy environment where quality measures and patient satisfaction ratings are becoming the basis for reimbursement rates, one wonders how VMS software is getting traction. Perhaps desperate times call for desperate measures, and the challenge of filling employment gaps is driving interest in impersonal digital match services? Rural hospitals are desperate to recruit quality candidates, and with a severe physician shortage looming, warm bodies are becoming an acceptable solution to staffing needs.
As distasteful as the thought of computer-matching physicians to hospitals may be, the real problems of VMS systems only become apparent with experience. After discussing user experience with several hospital system employees and reading various blogs and online debates here’s what I discovered:
1. Garbage In, Garbage Out. The people who input physician data (including their certifications, medical malpractice histories, and licensing data) have no incentive to insure accuracy of information. Head hunter agencies are paid when the physicians/nurses they enter into the database are matched to a hospital. To make sure that their providers get first dibs, they may leave out information, misrepresent availability, and in extreme cases, even falsify certification statuses. These errors are often caught during the hospital credentialing process, which results in many hours of wasted time on the part of internal credentialing personnel, and delays in filling the position. In other cases, the errors are not caught during credentialing and legal problems ensue when impaired providers are hired accidentally.
2. Limitation of choice. The non-compete contracts associated with VMS systems typically prevent hospital physician recruiters from contacting staffing agencies directly to fill their needs. This forces the hospital to rely on the database for all staffing leads. At least 68% of staffing agencies do not participate with VMS systems, so a large portion of the most carefully vetted professionals remain outside the VMS, inaccessible to those who contracted to use it.
3. Extra hospital employee training required. There are hundreds of proprietary VMS systems in use. Each one requires specialized training to manage everything from durable medical equipment to short term surgical staff. In cases where hospital staff are spread too thin to master this training, some VMS companies are pleased to provide a “managed service provider” or MSP to outsource the entire recruitment process. This adds additional layers, further removing the hospital recruiter from the physician.
4. Providers hate VMS systems. As anyone who has read a recent nursing blog can attest, VMS systems are universally despised by the potential employees they represent. VMS paints professionals in black and white, without the ability to distinguish quality, personality, or perform careful reference checks. They force down salaries, may rule out candidates based on where they live (travel costs), and provide no opportunity to negotiate salary vis-a-vis work load. When a hospital opts to use a VMS system as a middle man between them and the staffing agencies, the agencies often pass along the cost to the providers by offering them a lower hourly rate.
5. Provider privacy may be compromised. Once a physician or nurse curriculum vitae (CV) is entered into the VMS database the agency recruiter who entered it has 1 year (I can’t confirm that this is true for all systems) to represent them exclusively. After that, the CV is often available for any recruiter who has access to that VMS to view or pitch to any client. There is a wide variety of agency quality in the healthcare staffing industry, with some being highly ethical and selective in choosing their clients (only quality hospitals) and providers (carefully screened). Others are transactional, bottom-feeders with all the scruples of a used car salesman. When your data is in a VMS, one minute you might be represented by a caring, thoughtful recruiter who understands and respects your career needs, and the next (without your informed consent) you’ll be matched to a bankrupt hospital undergoing investigation by the Department of Health by a gum-chewing salesman who threatens you with a lawsuit if you don’t complete an assignment for half the pay you usually receive.
6. No cost savings, only increased liability. In the end, some hospitals who have tried VMS systems say that their decreased hiring costs have not resulted in overall savings. While they may see a downward shift in salary paid to their temporary work force, they get what they pay for. Just one “bad hire” who causes a medical malpractice lawsuit can eat up salary savings for an entire year of VMS. Not to mention the increased costs associated with a slower hiring process, attrition from poor fits, and the inconvenience of having to re-recruit for positions over and over again. Providers also lose out on career opportunities while they’re “on hold” during a prolonged hiring process. And for those who layer on a MSP, they lose control of the most important hospital quality and safety line of defense – choosing your own doctors and nurses.
In summary, while the idea of using a software matching service for recruiting physicians and nurses to hospitals sounds appealing at first, the bottom line is that reducing care providers to a group of numerical fields removes all the critical nuance from the hiring process. VMS, with their burdensome non-competes, cumbersome technology, and lack of quality control are an unwelcome new middle man in the healthcare staffing environment. It is my hope that they will be squeezed out of the business based on their own inability to provide value to a healthcare system that craves and rewards quality and excellence in its staff.
Job matching requires thoughtful hospital recruiters in partnership with ethical, experienced agencies. Choosing one’s hospital gauze vendor should involve a different selection algorithm than hiring a new chief of surgery. It’s time for physician and nurse groups to take a stand against this VMS-inspired commoditization of medicine before its roots sink in too deeply and we all become mere line items on a hospital vendor list. So next time you doctors and nurses plan to work a temporary assignment, ask your recruiter if they use a VMS system. Avoiding those agencies who do may mean a much better (and higher paying) work experience.
*Locum tenens (filling hospital staffing needs with part time or traveling physicians and nurses) is big business. Here is a run down of the estimated market size and its key industry leaders (provided by CompHealth):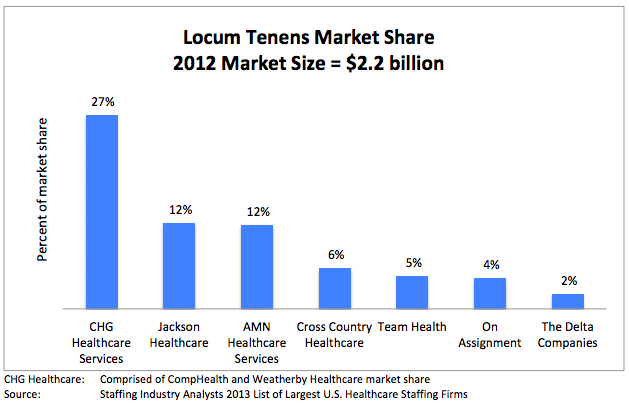
October 15th, 2013 by Dr. Val Jones in Expert Interviews
No Comments »
 I recently wrote about my experiences as a traveling physician and how to navigate locum tenens work. Today I want to talk about the client (in this case, hospital) side of the equation. I’ve had the chance to speak with several executives (some were physicians themselves) about the overall process of hiring and managing temporary physicians. What I heard wasn’t pretty. I thought I’d summarize their opinions in the form of a mock composite interview to protect their anonymity – I’m hoping that locum MDs and agencies alike can learn from this very candid discussion.
I recently wrote about my experiences as a traveling physician and how to navigate locum tenens work. Today I want to talk about the client (in this case, hospital) side of the equation. I’ve had the chance to speak with several executives (some were physicians themselves) about the overall process of hiring and managing temporary physicians. What I heard wasn’t pretty. I thought I’d summarize their opinions in the form of a mock composite interview to protect their anonymity – I’m hoping that locum MDs and agencies alike can learn from this very candid discussion.
Dr. Val: How do you feel about Locum Tenens agencies?
Executive: They’re a necessary evil. We are desperate to fill vacancies and they find doctors for us. But they know we are desperate and they take full advantage of that.
Dr. Val: What do you mean?
Executive: They charge very high hourly rates, and they don’t care about finding the right fit for the job. They seem to have no interest in matching physician temperament with hospital culture. They are only interested in billable hours and warm bodies, unfortunately. But we know this going in.
Dr. Val: Do you try to screen the candidates yourself before they begin work at your hospital?
Executive: Yes, we carefully review all their CVs and we interview them over the phone.
Dr. Val: So does that help with finding better matches?
Executive: Not really. Everyone looks good on paper and they sound competent on the phone. You only really know what their work ethic is like once they’ve started seeing patients.
Dr. Val: What percent of locums physicians would you say are “sub-par” then?
Executive: About 50%.
Dr. Val: Whoah! That’s very high. What specifically is wrong with them? Are they poor clinicians or what?
Executive: It’s a lot of things. Some are poor clinicians, but more commonly they just don’t work very hard. They have this attitude that they only have to see “X” number of patients per day, no matter what the census. So they’re not good team players. Also many of them have prima donna attitudes. They just swish into our hospital and tell us how they like to do things. They have no problem complaining or calling out flaws in the system because they know they can walk away and never see us again.
Dr. Val: Yikes, they sound horrible. Looking back on those interviews that you did with them, could you see any of this coming? Are there red flags in retrospect?
Executive: None that I can think of. All of our problem locums have been very different – some are old, some are young – they come from very different backgrounds, cultures, and parts of the country. I can’t think of anything they had in common on paper or in the phone interviews.
Dr. Val: So maybe the agencies don’t screen them well?
Executive: Right. I think they probably ignore negative feedback about a physician and just “solve the problem” by not sending them back to the same hospital. They just send them elsewhere – and so the problem continues. They have no incentive really to take a locums physician out of circulation unless they do something truly dangerous at work (medical malpractice). That’s pretty rare.
Dr. Val: I recently wrote on my blog that there are 4 kinds of physicians who do locums: 1. Retirees, 2. Salary Seekers, 3. Dabblers and 4. Problem personalities – would you agree with those categories?
Executive: Yes, but I think that a large proportion of the locums I’ve met have been either motivated by money (i.e. they want to make some extra cash so they can go on a fancy vacation) or they just don’t get along well with others. There are more “problem people” out there than you think.
Dr. Val: This is rather depressing. Have you found that some agencies do a better job than others at keeping the “good” physicians coming?
Executive: Well, we only work with 2 or 3 agencies, so I can’t speak to the entire range of options. We just can’t handle the complexity associated with juggling too many recruiters at once because we end up with accidental overlap in contracts. We have booked two doctors via two different agencies for the same block of time and then we are legally bound to take them both. It’s an expensive mistake.
Dr. Val: Does one particular agency stand out to you in terms of quality of experience?
Executive: No. Actually they all seem about the same.
Dr. Val: For us locums doctors, I can tell you that agencies vary quite a bit in terms of quality of assignments and general process.
Executive: There may be a difference on your end, but not much on ours.
Dr. Val: So, being that using locums has been a fairly negative experience for you, what do you intend to do to change it?
Executive: We are trying very hard to recruit full time physicians to join our staff so that we reduce our need for locums docs. It’s not easy. Full time physician work has become, quite frankly, drudgery. Our system is so burdened with bureaucratic red tape, decreasing reimbursement, billing rules and government regulations that it sucks the soul right out of you. I don’t like who I become when I work full time. That’s why I had to take an administrative job. I still see patients part-time, but I can also get the mental and emotional break I need.
Dr. Val: So you’re actually a functional locums yourself, if not a literal one.
Executive: Yes, that’s right. I have some guilt about not working full time, and yet, I have to maintain my sanity.
Dr. Val: Given the generally negative work environment that physicians live in these days, I suppose that temporary work is only going to increase exponentially as others take the path that you and I have chosen?
Executive: With the looming physician shortage, rural centers in particular are going to have to rely more and more on locums agencies. What agencies really need to do to distinguish themselves is hire clinicians to help them screen and match locums to hospitals. Agencies don’t seem to really understand what we need or what the problems are with their people. If they had medical directors or a chief medical officer, people who have worked in the trenches and understand both the client side and the locum side, they would be much better at screening candidates and meeting our needs. Until then, we’re probably going to have to limp along with a 50% miss-match rate.
August 22nd, 2013 by Dr. Val Jones in Health Policy, Opinion
3 Comments »
 I used to be a big believer in the transformative power of digital data in medicine. In fact, I devoted the past decade of my life to assisting the “movement” towards better record keeping and shared data. It seemed intuitive that breaking down the information silos in healthcare would be the first logical step in establishing price transparency, promoting evidence-based practices, and empowering patients to become more engaged in their care decisions. Unfortunately I was very wrong.
I used to be a big believer in the transformative power of digital data in medicine. In fact, I devoted the past decade of my life to assisting the “movement” towards better record keeping and shared data. It seemed intuitive that breaking down the information silos in healthcare would be the first logical step in establishing price transparency, promoting evidence-based practices, and empowering patients to become more engaged in their care decisions. Unfortunately I was very wrong.
Having now worked with a multitude of electronic medical records systems at hospitals around the country, one thing is certain: they are doing more harm than good. I’m not sure that this will change “once we get the bugs out” because the fundamental flaw is that electronic medical records require data entry and intelligent curation of information, and that becomes an enormous time-suck for physicians. It forces us away from human interaction, thus reducing our patients’ chances of getting a correct diagnosis and sensible treatment plan.
How bad is it? The reality on the ground is that most hospitals are struggling enormously with EMR implementation. There are large gaps in the technology’s ability to handle information transfer, resulting in increased costs in the hundreds of millions of dollars per small hospital system, not to mention the tragically hilarious errors that are introduced into patient records at break neck pace.
At one hospital, the process for discharging a patient requires that the physician type all the discharge summary information into the EMR and then read it into a dictation system so that it can be transcribed by a team in India (cheaper than US transcription service) and returned to the hospital in another part of the EMR. The physician then needs to go into the new document and remove all the typos and errant formatting so that it resembles their original discharge summary note. In one of my recent notes the Indian transcriptionist misheard my word for “hydrocephalus” and simply entered “syphilis” as the patient’s chief diagnosis. If I hadn’t caught the error with a thorough reading of my reformatted note, who knows how long this inaccurate diagnosis would have followed the poor patient throughout her lifetime of hospital care?
Another hospital has an entire wing of its main building devoted to an IT team. I accidentally discovered their “Star Trek” facility on my way to radiology. Situated in a dark room surrounded by enough flat panel monitors to put a national cable network to shame, about 40 young tech support engineers were furiously working to keep the EMR from crashing on a daily basis – an event which halts all order processing from the ER to the ICU. Ominous reports of the EMR’s instability were piped over the entire hospital PA system, warning staff when they could expect screen freezes and data entry blockages. Doctors and nurses scurried to enter their orders and complete documentation during pauses in the network overhaul. It was like a scene from a futuristic movie where humans are harnessed for work by a centralized computer nexus.
At yet another hospital, EMR-required data entry fields regularly interrupt patient throughput. For example, a patient could not be given their discharge prescriptions without the physician indicating (in the EMR) whether each of them is a tablet or a capsule. As patients and their family members stand by the nursing desk, eager to be discharged home, their physician is furiously reviewing their OTC laxative prescriptions trying to click the correct box so that the computer will allow the transfer of the entire prescription list to the designated pharmacy. When I asked about the insanity of this practice, a helpful IT hospital specialist explained that the “capsule vs tablet” field was required by Allscripts in order to meet interoperability requirements with our hospital’s EMR. This one field requirement probably resulted in hundreds of extra hours of physician time per day throughout the hospital system, without any enhancement in patient care or safety.
For those of you EMR evangelists in Washington, I’d encourage you to take a long, cold look at what’s happening to healthcare on the ground because of these digital data initiatives. My initial enthusiasm has turned to exasperation and near despondency as I spend my days as a copy editor for an Indian transcription service, trying to prevent patients from being labeled as syphilitics while worrying about whether or not the medicine they’re taking is classified as a tablet or a capsule in a system where I may not be able to enter any orders at all if the central tech command is fixing software instability in the Star Trek room.
December 26th, 2011 by Debra Gordon in Opinion
No Comments »
One of the hot phrases in health care these days is “patient-centered,” as in “patient-centered hospitals,” “patient-centered practices,” and “patient-centered medicine.” For all of you out there working on creating such “patient-centered” systems, let me provide a bit of advice based on a recent experience my family and I had with Delta Airlines. For if you substitute the word “customer” for “patient,” you get what every business, whether in health care or not, should be focused on — the person receiving, nay, purchasing, their services. The ones you hope will return, again and again.
I’m actually writing this as I sit in the lobby of a hotel in Park City, Utah. It is a gorgeous day outside, crisp and cold, just perfect for the skiing my family had in mind when we booked this trip; it’s a short trip– just 3 days on the slopes before we head home — so every minute counts. Unfortunately, despite plenty of time sitting in airports yesterday (i.e., no tight connection), only 2 out of our 6 pieces of luggage made it here. Fortunately, one of those was the suitcase filled with skiing togs. Unfortunately, one of the missing pieces was my son’s new snowboard, also filled with all of his ski togs. So while my boys are out on the slopes (the snowboard kid wearing my ski clothes), I’m sitting in the lodge awaiting our luggage. It is nearly noon — half of the day gone, one-sixth, possibly one-third, of our vacation gone–and I have not yet set foot on the slopes. Sure, I could head over and buy all-new ski stuff. . . . but that isn’t the point.
The point is how this was handled. Read more »
*This blog post was originally published at A Medical Writer's Musings on Medicine, Health Care, and the Writing Life*
 Electronic medical records (EMRs) now play a part in the daily documentation routine for most physicians. While improvements in access to patient data, legibility of notes, and ease of order entry are welcome enhancements, there is a significant downside to EMRs as well. Although I’ve blogged about my frustrations with nonsensical, auto-populated notes and error carry-forward, there is a more insidious problem with reliance on EMRs: digital dependency.
Electronic medical records (EMRs) now play a part in the daily documentation routine for most physicians. While improvements in access to patient data, legibility of notes, and ease of order entry are welcome enhancements, there is a significant downside to EMRs as well. Although I’ve blogged about my frustrations with nonsensical, auto-populated notes and error carry-forward, there is a more insidious problem with reliance on EMRs: digital dependency.

 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.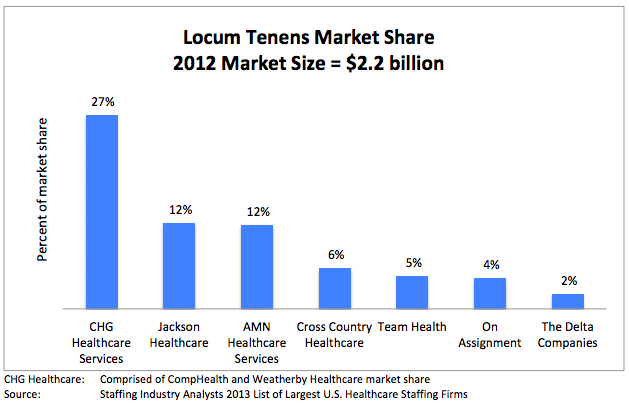
 I recently wrote about
I recently wrote about  I used to be a big believer in the transformative power of digital data in medicine. In fact, I devoted the past decade of my life to assisting the “movement” towards better record keeping and shared data. It seemed intuitive that breaking down the information silos in healthcare would be the first logical step in establishing price transparency, promoting evidence-based practices, and empowering patients to become more engaged in their care decisions. Unfortunately I was very wrong.
I used to be a big believer in the transformative power of digital data in medicine. In fact, I devoted the past decade of my life to assisting the “movement” towards better record keeping and shared data. It seemed intuitive that breaking down the information silos in healthcare would be the first logical step in establishing price transparency, promoting evidence-based practices, and empowering patients to become more engaged in their care decisions. Unfortunately I was very wrong.