November 9th, 2010 by GarySchwitzer in Better Health Network, Health Policy, News, Opinion
No Comments »

Take medical uncertainty. Add financial incentive to treat. Voila! Increased utilization. Now take away financial incentive to treat. Guess what you get?
MedPageToday explains, in the case of hormone therapy for prostate cancer:
Medicare accomplished what clinical guidelines and evidence-based medicine couldn’t: it reduced unnecessary use of androgen deprivation therapy (ADT) in prostate cancer.
Inappropriate use decreased by almost 30% from 2003 to 2005, following enactment of the Medicare Modernization Act, which lowered physician reimbursement for ADT. Appropriate use of ADT did not change during the same time period, according to an article in the Nov. 4 issue of the New England Journal of Medicine.
“Our findings suggest that reductions in reimbursement may influence the delivery of care in a potentially beneficial way, with even the modest [reimbursement] changes in 2004 associated with a substantial decrease in the use of inappropriate therapy,” Vahakn B. Shahinian, MD, of the University of Michigan in Ann Arbor, and co-authors wrote in conclusion.
“The corollary is that reimbursement policies should be carefully considered to avoid providing incentives for care for which no clear benefit has been established. The extreme profitability of the use of gonadotropin-releasing hormone (GnRH) agonists during the 1990s probably contributed to the rapid growth in the use of ADT for indications that were not evidence-based.”
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
July 28th, 2010 by Davis Liu, M.D. in Better Health Network, Health Policy, News, Opinion, Research
2 Comments »

 The American College of Obstetricians and Gynecologists (ACOG) recently reiterated their position that Pap smears should be performed on healthy women starting at age 21. This is different from the past which recommended screening for cervical cancer at either three years after the time a woman became sexually active or age 21, whichever occurred first.
The American College of Obstetricians and Gynecologists (ACOG) recently reiterated their position that Pap smears should be performed on healthy women starting at age 21. This is different from the past which recommended screening for cervical cancer at either three years after the time a woman became sexually active or age 21, whichever occurred first.
How will the public respond to this change?
Over the past year there have been plenty of announcements from the medical profession regarding to the appropriateness of PSA screening for prostate cancer and the timing of mammogram screening for breast cancer. Understandably, some people may view these changes in recommendations as the rationing of American healthcare. Read more »
*This blog post was originally published at Saving Money and Surviving the Healthcare Crisis*
June 8th, 2010 by Toni Brayer, M.D. in Better Health Network, Health Tips
No Comments »

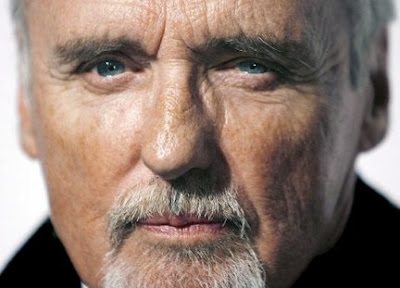 When Dennis Hopper died of prostate cancer at age 74, my husband asked me: “Hey, I thought prostate cancer is slow-growing and doesn’t kill men.”
When Dennis Hopper died of prostate cancer at age 74, my husband asked me: “Hey, I thought prostate cancer is slow-growing and doesn’t kill men.”
Well, he’s right about it usually being slow-growing, but prostate cancer is still the second leading cause of cancer death in men. His question made me realize that there are some facts that everyone should know about prostate cancer. Read more »
*This blog post was originally published at EverythingHealth*
September 16th, 2009 by DrRob in Better Health Network, Health Policy
No Comments »

I got something in my e-mail this morning. It’s a press release aimed at helping with prostate cancer awareness month, and is supported by Lance Armstrong’s foundation.
SURVEY SHOWS AT-RISK MEN LACKING IN PROSTATE CANCER KNOWLEDGE
SUNNYVALE, CALIF.,– September 9, 2009 – Prostate cancer remains one of the most commonly diagnosed cancers in the United States. In fact, one in six men will develop prostate cancer. It is also the second-leading cause of cancer death in the United States. But a recent survey suggests that many men at risk for the cancer still aren’t aware of all available treatment options. The survey, conducted late last year, reveals that nearly 50% of men aged 40 and older are not aware of the most common approach to surgery for prostate cancer — robotic-assisted surgery to remove the prostate. “I had to do my own research and then self-admit myself to the [hospital],” says surgery patient Tim Propheter. “…. Most people are just told … ‘Sorry, you have to have surgery, and we’ll set you up for such and such day,’ and they don’t know any better until they run into someone like me,” he says. This lack of information persists despite the fact that prostate cancer treatment has changed dramatically in the last decade. For example, surgery — which remains the gold standard treatment for localized prostate cancer — has become much less invasive. According to the American Urologic Association, the major benefit of prostatectomy, or prostate removal, is a potential “cancer cure” in patients with localized or early stage cancer.
Guess who the press release was from? Guess who sponsored the survey? The following was at the bottom of the email:
About the survey
Data was collected from 1000 self-selected adult healthcare information seekers through an online panel available through Ztelligence.com, using an survey questionnaire. Fifty-four percent of those were male and 46 percent were female. The results reflect only the opinions of the healthcare seekers who chose to participate.
About Intuitive Surgical, Inc.
The survey was conducted by Intuitive Surgical, Inc. (NASDAQ: ISRG), the manufacturer of the da Vinci Surgical System, the world’s only commercially available system designed to allow physicians to provide a minimally invasive option for complex surgeries. Intuitive Surgical, headquartered in Sunnyvale, California, is the global technology leader in robotic-assisted, minimally invasive surgery (MIS). Intuitive Surgical develops, manufactures and markets robotic technologies designed to improve clinical outcomes and help patients return more quickly to active and productive lives. The company’s mission is to extend the benefits of minimally invasive surgery to the broadest possible base of patients. Intuitive Surgical — Taking surgery beyond the limits of the human hand.™
Imagine that. A survey done by company that sells the da Vinci robotic surgical equipment shows that men have tragically no knowledge of the da Vinci robotic prostate surgery!
So let’s see what the evidence shows:
- Prostate cancer occurs in 186,000 men each year and kills nearly 29,000.
- In a well-known autopsy survey, over 1/3 of men over 80 were found to have cancer present in their prostate without evidence of significant disease. It is not clear how many of these men will progress to overt cancer, but it is very clear that this is the vast minority.
- PSA Testing (the blood test for prostate cancer screening) is by far the largest source of surgical candidates. It is a controversial test, having a high rate of false positives and an unproven record of significant benefit.
From the reference uptodate.com:
The European Randomized Study of Screening for Prostate Cancer (ERSPC) reported a small absolute survival benefit with PSA screening after nine years of follow-up; however, 48 additional patients would need aggressive treatment to prevent one prostate cancer death. Although the report did not address quality of life outcomes, considerable data show the potential harms from aggressive treatments. Further sustaining the uncertainty surrounding screening, a report from the large United States trial, the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, published concurrently with the European trial, found no benefit for annual PSA and digital rectal examination (DRE) screening after seven to ten years of follow-up. The crux of this screening dilemma was aptly stated by the urologist Willet Whitmore, who asked “is cure possible in those for whom it is necessary, and is cure necessary in those for whom it is possible?”
The most important line in this is at the end of the first sentence, stating that 48 patients would need aggressive treatment (including prostatectomy) to prevent one prostate cancer death. So how much does “aggressive treatment to prevent cancer death” cost?
From the Journal of Clinical Oncology:
For patients in the treatment-received analysis, the average costs were significantly different; $14,048 (95% confidence interval [CI], $13,765 to $14,330) for radiation therapy and $17,226 (95% CI, $16,891 to $17,560) for radical prostatectomy (P < .001). The average costs for patients in the intent-to-treat analysis were also significantly less for radiation therapy patients ($14,048; 95% CI, $13,765 to $14,330) than for those who underwent radical prostatectomy ($17,516; 95% CI, $17,195 to $17,837; P < .001).
note: it was very hard to find numbers here. This is actually from Medicare claims from 1992 and 1993, so it is a huge underestimate from today’s numbers.
Which means that based on the 1992 numbers, you would spend $672,000 to save one life using radiation therapy and $1,084,000 if you used surgery. This does not take into account the consequences of surgery for the men who underwent the surgery.
What about robotic surgery? In a comparison of the cost of open prostatectomy to robot-assisted surgery, the cost is even higher.
Cost was the one area in which the older open surgery was the clear winner: Open radical prostatectomy costs $487 less a case than non-robotic laparoscopy and $1,726 less than robot-assisted prostatectomy.
According to the review, “Shorter operative time and decreased hospital stays associated with the robotic procedure did not make up for the cost of the additional equipment expenditure.” Estimated costs of the robotic system to a provider run about $1.2 million a year, with maintenance costs of $120,000 a year and one-time costs of $1,500 a case.
To summarize:
- Prostate cancer screening is controversial, as it fails to differentiate between the minority of men who would die from the disease from the majority who would simply die with it.
- PSA Testing as greatly increased the number of men diagnosed with early stage cancers.
- Prostate cancer surgery or radiation therapy is recommended for men who have early stage cancers.
- Aggressive prostate cancer treatment has to be done 48 times to save one life.
- The most expensive treatment for prostate cancer is prostatectomy, or removal of the prostate.
- The robotic form of the surgery is a higher-cost procedure by a significant amount.
So, an expensive form of surgery that may not be appropriate is done on a group of men identified on a very unreliable test yielding a very small number of lives saved and a lot of men who then have to deal with the physical consequences of the surgery. Why in the world is this being promoted at all?
Money. Here’s the homepage of one of our local hospitals. They have aggressively marketed da Vinci surgery on television, billboards, and the radio.

Why do you think they would pay as much money as they do for this device? It’s good business? Not so fast. Dr. Paul Levy stated back in 2007 about this very procedure:
Here you have it folks — the problem facing every hospital, and especially every academic medical center. Do I spend over $1 million on a machine that has no proven incremental value for patients, so that our doctors can become adept at using it and stay up-to-date with the “state of the art”, so that I can then spend more money marketing it, and so that I can protect profitable market share against similar moves by my competitors?
No, hospitals are employing this just to keep pace. The real winner in this is Intuitive Surgical, Inc., who has been a darling of Wall Street, beating estimates in earnings with a Q2 net profit of $62.4 Million.
Why is the cost of healthcare going up while physician reimbursement goes down and hospitals go out of business?
It’s Intuitive.
God Bless America!



*This blog post was originally published at Musings of a Distractible Mind*
September 8th, 2009 by Dr. Val Jones in Health Tips, True Stories
No Comments »
 Ed Walker is 102 years old. I met him by chance on a steep hill in Lunenburg, Nova Scotia – not long after my husband blurted, “I hope you’ve got good brakes on that scooter!” Ed pulled up next to us (to demonstrate his brakes) and jubilantly announced his age, along with his suspected reason for it: “I have prostate cancer but chose to leave it alone.”
Ed Walker is 102 years old. I met him by chance on a steep hill in Lunenburg, Nova Scotia – not long after my husband blurted, “I hope you’ve got good brakes on that scooter!” Ed pulled up next to us (to demonstrate his brakes) and jubilantly announced his age, along with his suspected reason for it: “I have prostate cancer but chose to leave it alone.”
I chuckled to myself, thinking that he was probably right about his longevity-hospital avoidance connection.
Of course, the diagnosis and treatment of prostate cancer is being hotly debated these days. While no one likes the idea of leaving cancer untreated, slow-growing prostate cancer may be less of a threat to men at a certain age than the treatment required to cure it. And that’s a difficult truth to accept – especially for Americans.
My fellow blog contributors have noted the disconnect between scientific evidence and clinical practice in regards to prostate cancer. According to a recent study in the New England Journal of Medicine, PSA (a screening test for prostate cancer) testing has not made a difference in overall longevity. Urologists still favor testing (the American Urological Association guidelines recommend initiating PSA testing for all men starting at age 40) while family medicine physicians don’t usually recommend it. Is there a conflict of interest driving this difference in recommendation? Perhaps – though I suspect it has more to do with a surgical mentality (to cut is to cure!) than a conscious decision to protect one’s income. If you think there’s a shortage of urologic procedures to go around, then I’d recommend you simply consider the increasing age of the US population. It’s not as if the prostate gland is the only thing that needs work “down there.”
Perhaps Americans can take some cues from their elderly neighbors to the north – and try to accept that doing something is not always better than “doing nothing.” In the case of some prostate cancers, it’s cheaper, safer, and a lot less painful.
Just ask Ed Walker.






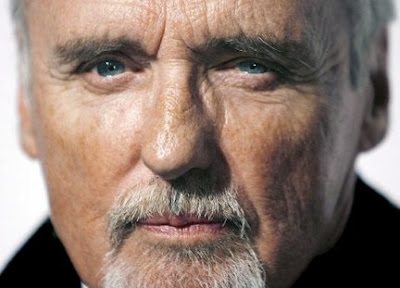 When Dennis Hopper died of prostate cancer at age 74, my husband asked me: “Hey, I thought prostate cancer is slow-growing and doesn’t kill men.”
When Dennis Hopper died of prostate cancer at age 74, my husband asked me: “Hey, I thought prostate cancer is slow-growing and doesn’t kill men.”










