January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
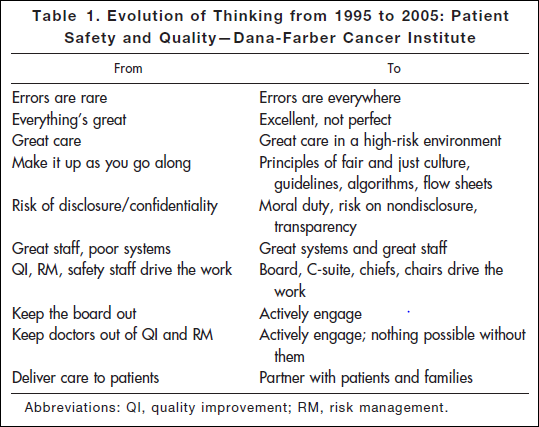
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
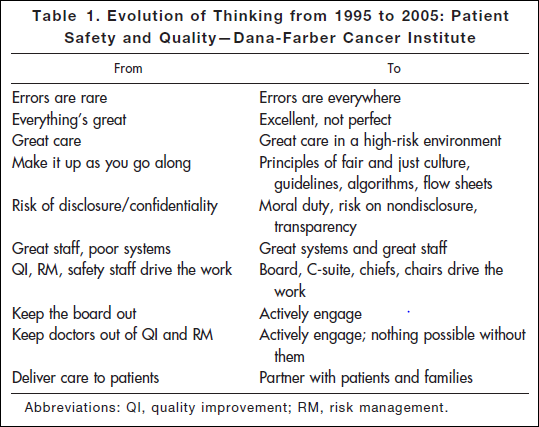
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*
December 29th, 2010 by eDocAmerica in Better Health Network, Opinion
No Comments »

Recently, I was involved in a discussion on an email list serve and decided to takes some of my comments on patient autonomy and blog about them. This arose following a debate about whether the term “patient” engendered a sense of passivity and, therefore, whether the term should be dropped in favor of something else, like “client” or something similar.
Having participated in the preparation and dissemination of the white paper on e-patients, I don’t see the need for “factions” or disagreements in the service of advancing Participatory Medicine. As Alan Greene aptly stated: “This is a big tent, with room for all.”
I want all of my patients to be as autonomous as possible. In my view, their autonomy is independent of the doctor-patient relationship that I have with them. They make the choice to enter into, or to activate or deactivate, the relationship with me. They may ignore my input, seek a second opinion, or fire me and seek the care of another physician at any time. They truly are in control in that sense. The only thing I have control over and am responsible for is trying to provide the best advice or consultation I can. Read more »
*This blog post was originally published at eDocAmerica*
December 15th, 2010 by Michael Sevilla, M.D. in Better Health Network, News, Opinion, True Stories
No Comments »

 My professional organization recently asked me to participate in an interesting meeting at the state capitol talking about healthcare payment reform and how to improve the healthcare delivery system. This was sponsored by the state of Ohio and their Health Care Coverage and Quality Council.
My professional organization recently asked me to participate in an interesting meeting at the state capitol talking about healthcare payment reform and how to improve the healthcare delivery system. This was sponsored by the state of Ohio and their Health Care Coverage and Quality Council.
It was the first meeting that I’ve been to where there were physicians, hospitals, insurance companies, and patients — all trying to put our heads together — present our points of view and try to come to consensus. Did we come to consensus on solutions? Not really, only that we will continue the conversation. There is no perfect solution that will make everyone happy, but we will strive to try to get to that best imperfect solution.
When is comes to healthcare delivery and healthcare payment, there was a lot of discussion on physicians and hospitals — meaning healthcare providers. The motivating factor in these cases uses terms like payment, lack of payment, incentives, bonuses, and penalties. Read more »
*This blog post was originally published at Doctor Anonymous*
December 15th, 2010 by admin in Health Tips
No Comments »
This is a guest post from Dr. Mary Lynn McPherson.
**********
Rescuing Patients On Darvon Or Darvocet With Zero Tolerance For Pain
On November 19, 2010 the Food and Drug Administration (FDA) called for a halt in the use of the popular opioid pain relievers Darvocet and Darvon. These products contain the opioid propoxyphene, and it has been used to treat mild to moderate pain for over 50 years. However, concerns have long been raised about the effectiveness of this drug, and the risk of death (accidental and suicide). Darvon and Darvocet were banned in Britain in 2005, followed by the European Union in 2009. Over the past 30 years, the FDA has received numerous petitions to take these drugs off the U.S. market.
Research has shown that Darvon and Darvocet are no more effective for treating moderate pain than over the counter drugs like acetaminophen, aspirin or ibuprofen. Unfortunately, Darvon and Darvocet cause a lot more side effects such as dizziness, drowsiness, nausea and vomiting, hallucinations and constipation (all pretty typical of opioids used to treat pain). But, the side effects don’t stop there. The data is in, and it’s not a pretty picture. A recent study requested by the FDA showed that when used at the recommended doses, Darvon and Darvocet cause significant changes in the electrical activity of the heart, which can lead to a fatal irregularity in your heartbeat, even after only short-term use.
Among those advocating for the removal of these drugs from the market were pharmacists. The American Society of Health-System Pharmacists approved a policy in 2007 advocating for the withdrawal of Darvon and Darvocet from the U.S. market, and recently testified at the FDA Advisory Committee to this effect. As an often overlooked member of the medical team, pharmacists have a vital role to play in providing safe and effective treatments. We serve as the last line of defense against improper or unwise prescribing of drugs — especially those for pain. We are drug experts, and we can help patients and doctors switch from Darvon or Darvocet to safer and more effective treatments. Read more »
December 14th, 2010 by BarbaraFicarraRN in Better Health Network, Health Tips, True Stories
1 Comment »

In a recent post I wrote why patients are the most important part of the medical team, and my colleagues, Elizabeth Cohen, Kevin Pho, MD, Donna Cryer, JD, and Carl R. Sullivan, MD, shared their insights as well. Today, Ginger Vieira, a patient living with type 1 diabetes and celiac disease, says:
“You, as the patient, are the most important part of the medical team because you are the one who makes the daily decisions, who balances your disease around dinners, soccer games, long hours at work without enough time to check your blood sugar and eat lunch. You are the one who takes the knowledge you learn from your doctor and fits it into your everyday life. That’s a huge role, and it’s never easy.”
 Ginger Vieira shares her story about the challenges and how her positive attitude is allowing her to lead a life she thought was off limits.
Ginger Vieira shares her story about the challenges and how her positive attitude is allowing her to lead a life she thought was off limits.
Contagious Confidence, Endless Possibilities
By Ginger Vieira
“Don’t let anyone tell you that you can’t do something.” My twin brother, Pete, said this to me several months ago. I wrote it down on an index card and taped it to my bathroom mirror. Funny thing is, it’s never been other people telling me I can or cannot do something. The loudest voice I hear is my own.
When I was diagnosed with type 1 diabetes in the seventh grade over eleven years ago, the first list that ran through my head was the list of things I probably couldn’t do anymore. I couldn’t eat ice cream without first counting the grams of carbohydrates in the bowl and determining how much insulin I needed. I couldn’t play basketball anymore (at least, that’s what I thought). I couldn’t buy candy and popcorn with my friends when we go to the movies without feeling overwhelmingly guilty about eating such diabetic-off-limits food. The list of foods, activities, dreams and goals I thought were off-limits seemed endless. Read more »
*This blog post was originally published at Health in 30*





 My professional organization recently asked me to participate in an interesting meeting at the state capitol talking about healthcare payment reform and how to improve the healthcare delivery system. This was sponsored by the state of Ohio and their
My professional organization recently asked me to participate in an interesting meeting at the state capitol talking about healthcare payment reform and how to improve the healthcare delivery system. This was sponsored by the state of Ohio and their 
 Ginger Vieira shares her story about the challenges and how her positive attitude is allowing her to lead a life she thought was off limits.
Ginger Vieira shares her story about the challenges and how her positive attitude is allowing her to lead a life she thought was off limits.







