November 17th, 2014 by Dr. Val Jones in News, Research
4 Comments »

A Cost Effective Fitness Band
In a new study published in the Annals of Internal Medicine, researchers found that overweight and obese patients who used a popular smart phone app (MyFitnessPal) did not lose significant weight after a 6 month trial period. The randomized controlled trial is the first of its kind to demonstrate that well-liked mobile apps may be ineffective for most users.
Two hundred and twelve racially diverse (73% female) patients treated at two UCLA primary care clinics were enrolled in the study. All indicated that they were interested in losing weight and 79% who completed the study indicated that they were “somewhat” or “completely” satisfied with the app, while 92% reported that they’d recommend it to a friend.
Unfortunately, as pleased as the subjects were with the app, there was no statistically significant difference in weight loss between the intervention and control groups. On average, the MyFitnessPal users lost 0.66 lbs in 6 months.
The authors note:
“Most participants rarely used the app after the first month of the study… Given these results it may not be worth a clinician’s time to prescribe MyFitnessPal to every overweight patient with a smart phone… Our analysis did not show any demographic covariates to be important predictors of app use.”
This study serves as a reminder that “popular” and “effective” do not always go hand-in-hand when it comes to weight loss interventions. While mHealth apps are expected to earn $26 billion by 2017, one is left to wonder if this money will be well spent or if we’ll all be “somewhat to completely satisfied” with the apps without anything medically significant to show for it?
November 13th, 2012 by Dr. Val Jones in Announcements, Celebrity Interviews
No Comments »
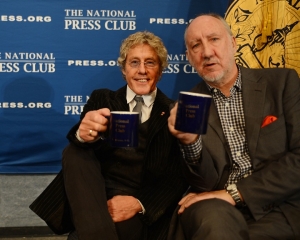
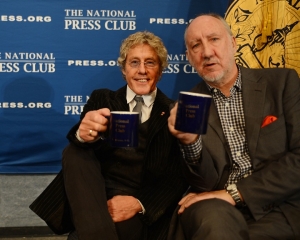 Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.
Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.
Sarah told the crowd what it was like to be a fifteen-year-old in a pediatric oncology unit populated by ukulele-playing clowns and screaming infants. The extreme age-related disconnect between her pscho-social needs and that of younger kids and babies served to make her feel even more isolated during her course of treatment. She longed for the companionship of others like her, but without any national cancer centers focused on the special needs of teens, she was on her own.
Roger Daltrey became interested in teen cancer when his personal physician took up the cause in the U.K. and turned to him for support. Daltrey’s decades of playing music to teen audiences made him keenly aware of their unique psycho-social needs. “When you’re a teenager, it’s horrifying if you have a spot on your nose. Imagine what it’s like if you have cancer!” said Daltrey.
Teen Cancer America began as a movement called the Teen Cancer Trust in the U.K. According to Daltrey, preliminary research (comparing teens treated in a typical NHS cancer ward versus a unit sponsored by the Teen Cancer Trust) suggests that there may be as much as a 15% survival advantage in being treated in the special units. Daltrey attributes this to increased morale that helps teens and families find the will to fight through life-threatening treatments.
When asked how American cancer centers compare to those in the U.K. Daltrey immediately responded that he believed the U.S. centers were far superior. He described the incredible resources available at UCLA and Duke, and how the facilities themselves were unbelievably beautiful, sporting plant-filled atria, massive skylights, and high tech imaging and radiation equipment. Nonetheless, he noted, “Teens don’t want to hang out in an atrium. There is just no place that appeals to teenagers at these centers.”
Whether specialized teen cancer treatment environments in the U.S. will dramatically improve survival rates remains to be seen, but there’s no doubt that recognizing the unique psycho-social needs of teenagers would be a boon for patients and families at pediatric cancer centers. Like post-traumatic stress disorder in military personnel, the psychological ravages of cancer may well be under recognized, especially in the teen and young adult populations.
Thank you Roger Daltry and Pete Townshend for bringing this to our attention.
***
Find out how to support Teen Cancer America here.
Check out The Who themed cookie from the press club event (delicious!):

August 10th, 2012 by Dr. Val Jones in True Stories
3 Comments »
 Dr. Pauline Chen recently wrote an interesting, if not slightly sterile, article about the prevalence of bullying in medical school. A survey published by JAMA in 1990 suggested that 85% of medical students had experienced some kind of mistreatment during their third year of training, and a quarter of the respondents said that they would have chosen a different profession had they known in advance about the extent of mistreatment they would experience.
Dr. Pauline Chen recently wrote an interesting, if not slightly sterile, article about the prevalence of bullying in medical school. A survey published by JAMA in 1990 suggested that 85% of medical students had experienced some kind of mistreatment during their third year of training, and a quarter of the respondents said that they would have chosen a different profession had they known in advance about the extent of mistreatment they would experience.
One medical school (UCLA) took these sobering statistics to heart and implemented an anti-bullying program of sorts. Thirteen years after it was initiated, more than half of all medical students still said that they had been intimidated or physically or verbally harassed.
I recently wrote a fairly tongue-in-cheek blog post about why doctors are jerks. But I didn’t really delve into the more sinister side of the bullying culture. Some of my experiences in medical training were soul-suckingly bad, and just to add some flavor to Dr. Chen’s analysis, let me share some real-life anecdotes.
My worst experiences in medical training occurred during Ob/Gyn rotations. I don’t know if this has been the experience of other medical students, or if my gender had anything to do with it, but I spent time with a group of female residents who were so toxic to med students that the department chairman actually warned us about them ahead of time in a private meeting. He let us know that these residents had a history of “hazing” medical students, particularly females. I had always been a very conscientious and hard working student, so I presumed that they wouldn’t have much to criticize. My plan was to work hard, keep my head down, and get out unscathed. Unfortunately, nothing went as planned.
The tone was set for me the first day when I witnessed a female, Asian anesthesia resident slap a pregnant Hispanic woman who was in labor. The woman was frightened and spoke no English and was beginning to hyperventilate from pain. The resident was trying to put in an epidural anesthetic and the woman was moving around too much for her to get the needle safely into position. So instead of calling for a translator, the resident started raising her voice, eventually screaming at the woman to calm down. The woman was crying uncontrollably, so the resident slapped her, and told her that she was “going to lose her baby” if she didn’t shut up. The husband was also terrified and could understand some English. He translated to his wife that she was going to lose the baby and started begging her to be calm. I stood in the doorway with my mouth open. The resident told me to get the f-out of there as she threw her gloves at me.
I suppose the humiliation of being caught abusing a patient was enough to channel her hate towards me, so she told the Ob/Gyn residents that I was an incompetent medical student. For the rest of the month I was targeted by the hazing team, and like a pack of wolves they descended, bound to make my every moment a living hell. During the delivery of my first baby (a touching experience that moved me to tears), the new mom experienced a small tear during the birthing process. The residents blamed it on me, and convinced me that I had personally caused her harm by not “supporting her perineum” correctly. I was mortified and fell for the lie – hook, line, and sinker.
When a woman went into labor it was customary for the residents to page the medical student on call and have him or her assist with the vaginal birth or c-section. My peers were paged in a timely manner, while I was either paged at random times or paged to the wrong parts of the hospital so that I appeared to be late to several deliveries (especially when a senior physician evaluator was present to witness it). Once I caught on to this I had to remain awake 24/7 at the nursing station (rather than the more secluded med student lounge) so that I could follow visual cues regarding where and when to assist. After several shifts without sleep the residents began locking the chairs in their lounge so that I would have no where to sit or rest, but would be forced to remain standing “on guard” all night.
One page was particularly painful at the time (but almost laughable in retrospect). A resident took it upon herself to page me just to tell me some important news: I was the worst medical student in the history of the program.
Of course, my final resident evaluation was dripping with venom. I recall statements such as, “Valerie suffers from narcolepsy,” and “she is uniformly late and is never prepared… she doesn’t answers her emergency pages… she occupies valuable space at the nursing station instead of remaining in the medical student on-call room… her performance in deliveries borders on dangerous.” And on it went. I wish I had the maturity to take all of that in stride at the time and see that these women were nuts, and it had nothing to do with me personally. But I was too close to it then, and I bore the pain with a stiff upper lip.
I still think about that poor patient who was slapped, and I kick myself for not standing up to the resident who hit her. I guess I was in such shock that I didn’t know what to do. But living through this abuse helped me to become a stronger patient advocate during my residency years. Just two years after my brush with the Ob/Gyn residents, I gained a reputation for being the intern you never f-with. I know I saved the lives of some who were slipping through the cracks of the system, and I was willing to call in the hospital ethics committee if I had to. Yes, that pregnant woman’s suffering was not totally in vain – because she helped me to find my own cojones. And for that, I will always be grateful.
December 21st, 2011 by HarvardHealth in Health Tips, News
No Comments »

The word “cancer” strikes fear in everyone who is told they have it. It conjures up images of a fast-moving, life-threatening disease.
That isn’t necessarily the case for men with newly diagnosed prostate cancer. More than half of them have a type of cancer that is confined to the prostate gland and that grows so slowly it will never affect their health or their lives. Yet almost 90% of men told they have prostate cancer opt for immediate treatment with surgery or radiation therapy—which often cause trouble getting or keeping an erection and an assortment of urinary problems.
Two weeks ago, a panel of experts convened by the National Institutes of Health recommended that many men with localized, low-risk prostate cancer be closely monitored, and that treatment be delayed until there was evidence that the disease was progressing.
“It’s clear that many men would benefit from delaying treatment,” Dr. Patricia A. Ganz, conference panel chairperson and director of the Division of Cancer Prevention and Control Research at the Jonsson Comprehensive Cancer Center at the University of California in Los Angeles, said in a statement, adding that Read more »
*This blog post was originally published at Harvard Health Blog*
September 10th, 2011 by Medgadget in Research
No Comments »

 Packing hearts on ice destined for transplantation may eventually become a thing of the past. The Organ Care System from TransMedics, which delivers a still-beating heart to a transplant patient, continues to show promise in clinical trials. UCLA recently reported that Rob Evans, a 61-year-old patient suffering from cardiomyopathy, is the most recent recipient of a heart delivered by the device.
Packing hearts on ice destined for transplantation may eventually become a thing of the past. The Organ Care System from TransMedics, which delivers a still-beating heart to a transplant patient, continues to show promise in clinical trials. UCLA recently reported that Rob Evans, a 61-year-old patient suffering from cardiomyopathy, is the most recent recipient of a heart delivered by the device.
We’ve actually covered the Organ Care System (OCS) several times before (we first caught wind of it in 2006). The device, however, is still classified as an investigational device by the FDA; it is undergoing phase II clinical trials in the United States at three sites: the Ronald Reagan UCLA Medical Center, the Cleveland Clinic, and New York-Presbyterian, Columbia University Medical Center.
Check out the UCLA press release explaining the technology and its use in the university’s Heart Transplant Program: Read more »
*This blog post was originally published at Medgadget*




 Dr. Pauline Chen recently wrote an interesting, if not slightly sterile,
Dr. Pauline Chen recently wrote an interesting, if not slightly sterile,

 Packing hearts on ice destined for transplantation may eventually become a thing of the past. The Organ Care System from TransMedics, which delivers a still-beating heart to a transplant patient, continues to show promise in clinical trials. UCLA recently reported that Rob Evans, a 61-year-old patient suffering from cardiomyopathy, is the most recent recipient of a heart delivered by the device.
Packing hearts on ice destined for transplantation may eventually become a thing of the past. The Organ Care System from TransMedics, which delivers a still-beating heart to a transplant patient, continues to show promise in clinical trials. UCLA recently reported that Rob Evans, a 61-year-old patient suffering from cardiomyopathy, is the most recent recipient of a heart delivered by the device.







