September 1st, 2015 by Dr. Val Jones in Book Reviews
1 Comment »
 I’m often asked to do book reviews on my blog, and I rarely agree to them. This is because it takes me a long time to read a book – and then if I don’t enjoy it, I figure the author would rather me remain silent than publish my true thoughts. Most of the reviews that I end up writing are unsolicited, but today is an unusual exception. A colleague asked me to read her book, “How To Be A Rock Star Doctor.” I got half way through when she checked in to see how things were going. I had to tell her that I didn’t agree with some of her advice to young doctors, and I worried that she would be discouraged by my honesty.
I’m often asked to do book reviews on my blog, and I rarely agree to them. This is because it takes me a long time to read a book – and then if I don’t enjoy it, I figure the author would rather me remain silent than publish my true thoughts. Most of the reviews that I end up writing are unsolicited, but today is an unusual exception. A colleague asked me to read her book, “How To Be A Rock Star Doctor.” I got half way through when she checked in to see how things were going. I had to tell her that I didn’t agree with some of her advice to young doctors, and I worried that she would be discouraged by my honesty.
I was very pleasantly surprised to find that she welcomed the criticism and actually asked me to write my review – favorable or unfavorable as I saw fit. She is the very first author to take that position (others have thanked me for not writing a review) and I am proud of her for it.
In essence, How To Be A Rock Star Doctor, is an easy-to-read primer for young primary care physicians looking to setup their first outpatient practice. The troubling part of the book (for me) was Dr. Bernard’s approach to the empathy fatigue that can set in for overworked physicians. In her view, we must “fake it” if we’ve lost it or don’t have it.
The book contains specific advice for how to appear empathic. Smiling broadly (no matter how one is feeling internally), dressing in a white coat, and exuding confidence, are recommended because we should see our patient interactions as an acting role – we are on stage, and they are depending on us to look/act the part.
Although Dr. Bernard rightly points out that there is research to support smiling as a means to achieving a happier mood, I was left with a certain uneasiness about the idea of putting on an act for patients. Something about the potential for dishonesty didn’t feel right to me. But then again, maybe the alternative – just being oneself – can create a poor therapeutic relationship if we’re in a bad mood for some reason.
I have heard many times that doctors can be uncaring to patients. Heck, I’ve even blogged about terrible interactions that I’ve had with my peers when I was in the patient role. But what is the solution? Should doctors learn how to imitate the qualities of a compassionate physician to achieve career success, or should we go a little deeper and actually try to be caring and let the behavior flow from a place of sincerity?
On the one hand, any tips to make the doctor-patient relationship go more smoothly should be welcomed… but on the other, if patient care is just an act, then what kind of meaning do our relationships have? If we act empathic do we eventually become empathic? Maybe yes, maybe no.
One thing I’m sure of, Dr. Bernard has opened an interesting discussion about how to handle stress, burnout, and create an excellent therapeutic experience in the midst of a broken healthcare system. She is willing to take criticism, and has endeared herself to me through our email exchanges. While I may not agree with all of her strategies to optimize patient satisfaction, one thing seems clear: she is as advertised — a rock star doctor.
Check out her book and find your own path forward. 🙂
August 28th, 2015 by Dr. Val Jones in Health Tips, True Stories
1 Comment »

A Cat Playing Whack-A-Mole
Medication non-adherence is a hot button topic in healthcare. Physicians lament patient “non-compliance” with their medical advice, and policy wonks tell us that more than half of patients do not take their medications as directed. Missed opportunities to control chronic illnesses such as diabetes, heart disease, and cancer surely do cost us untold billions of dollars and millions of quality life years lost annually in the U.S. But there is a flip side to the equation that no one is talking about. The costs of polypharmacy (over medication).
In my opinion, many Americans, especially those over 65, are taking far too many medicines. The unwanted side effects and medication interactions (both known and unknown) can be devastating. In my line of work (inpatient rehabilitation) I receive a steady stream of patients who have fallen and injured themselves or have been involved in serious accidents. An astonishing number of these incidents are related to drug side effects.
Take, for example, the elderly woman who had mild hypertension. Unbeknownst to her physicians, she was not compliant with the diuretics she had been prescribed. Each successive visit it was presumed that she was taking her medicines as directed, and that they were not sufficient to control her blood pressure. So the dosing was increased. Her husband dutifully picked up the new prescriptions from the pharmacy, and she collected them (unopened) in her desk drawer.
One day this spirited lady caught pneumonia and required a couple of days of inpatient monitoring and antibiotics at the local hospital. Her son decided to assist with her transition back home and stayed with her for a week, taking on both cooking and medication administration duty from his dad. He found all of her pills in her desk drawer and began to give them to her as directed.
Several days later the distraught son told me that his mother’s health had taken a nose-dive, and that she was hallucinating and acting uncharacteristically hostile. He took her to a more distant specialty hospital, where their initial impression was that she had advanced dementia, which had probably gone unnoticed by a son who hadn’t lived nearby for years. She would benefit from hospice placement.
The reality was, of course, that this poor woman was as dehydrated as a raisin and was becoming delirious from excessive diuretic use. Once I figured out that her son’s sudden, and very well-intentioned, medication adherence program was to blame, we stopped the blood pressure medications, gave her some water and she returned to her usual self within 24 hours.
On another occasion, I admitted a closed-head injury patient who had lost her front teeth after fainting and falling head first onto the asphalt in a grocery store parking lot. This was her third head injury in 6 months. A review of her medications revealed no less than six medications (that she was dutifully taking for various diseases and conditions) that carried a known side-effect of “dizziness.” We were able to discontinue all of them, and to this day I have not heard of another fall.
Just last week a wise, elderly patient of mine declined to take her blood pressure medicine. I explained to her that her blood pressure was higher than we’d like and that I wanted to protect her from strokes with the medicines. She smiled kindly at me and said, “I know my body, and I get dizzy when my blood pressure is at the levels you doctors like. The risk of my falling and hurting myself when I’m dizzy is greater than the benefit of avoiding a stroke. I’ve been running at this blood pressure for 80 years. Let’s leave it be.”
What I’ve learned is that although there are costs to not taking medicines, there are costs to taking them too. It is hard to say how many injuries are accidentally prevented by patient non-adherence. But we all need to take a closer look at what’s in our desk drawers, and pare down the prescriptions to the bare minimum required. I consider it a great victory each time I reduce the number of medications my patients use, and I would urge my peers to join me in the pharmaceutical whack-a-mole game that is so sorely needed in this country.
***
The American Geriatrics Society provides a helpful list of medications that should be avoided whenever possible in older individuals.
August 25th, 2015 by Dr. Val Jones in Health Tips
1 Comment »
 This post originally appeared on The Barton Blog.
This post originally appeared on The Barton Blog.
It’s both expensive and time-consuming to obtain temporary coverage for a hospital or medical practice. Locum tenens clients have every right to expect high-quality care from the locum tenens providers they hire; but even the very best locums may not perform to their full potential if their onboarding isn’t carefully planned.
As a locum tenens physician with licenses in 14 states, I have much experience with the onboarding process. Here are 12 tips for facilities eager to encourage smooth transitions, foster good provider relationships, and provide excellent patient care.
1. Arrange for provider sign-outs.
Since lapses in provider communication is a leading cause of medical errors, you can protect your patients by organizing a face-to-face (or phone call) report between the current provider and the locum who is going to be assigned to their census. Studies have shown a 30% decrease in error rate when physicians hand off their patient panel in person.
2. Allow for at least one day of training overlap, if possible.
The incoming provider will adapt best to your unique environment and care process if he or she has the chance to “shadow” the current provider for a day. Various questions will naturally arise and be answered during real-time patient care. In emergency fill situations, this will obviously not be possible; but it will help ease transitions in cases where it can be done.
3. Get your IT ducks in a row before the locum tenens provider arrives.
Electronic medical records (EMR) systems are difficult to master, and attempting to learn how to navigate in a new one (or newer version of one) in the middle of a full patient caseload is a recipe for disaster. Logins and passwords should be set up long before the locum tenens provider arrives. EMR training needs should be discussed and planned for in advance. If an IT professional is available to sit with the locum during his or her first round of documentation attempts, so much the better.
4. Plan for a day or half-day of orientation.
A facility tour, combined with an in-person meeting of key hospital players, is extremely important. The following people should be included:
- Unit medical director
- Nursing and therapy supervisors
- Risk management staff
- Human resources
- Medical records staff
- Coding and billing staff
- Pharmacy staff
- Laboratory staff
5. Prepare a welcome packet in advance.
This packet should include important information about the organization, the assignment, and the facility, including:
- Site maps
- Parking instructions
- Orientation day schedule
- Door key codes (if applicable)
- ID badge instructions
- EMR login and password
- Dictation codes
- Cafeteria location and hours
- A hospital directory with key phone numbers highlighted
Make sure the locum knows who signs their time sheets and where their office is located. A coding “cheat sheet” may also be appreciated.
6. Invite the locum tenens provider to lunch or dinner at some point during their assignment.
This is a friendly way to show that you appreciate them, and you want to get to know them. Being on the road can be lonely, and most locums appreciate opportunities to socialize.
7. …
– See more at: http://www.bartonassociates.com/2015/08/18/12-ways-to-help-your-locum-tenens-provider-succeed/#sthash.6KV0S3vE.dpuf
August 17th, 2015 by Dr. Val Jones in True Stories
26 Comments »
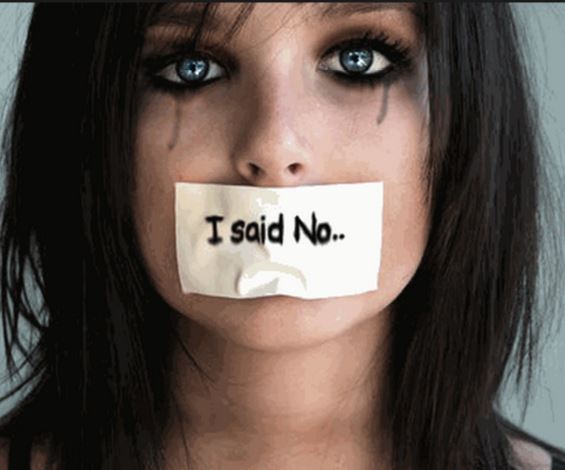
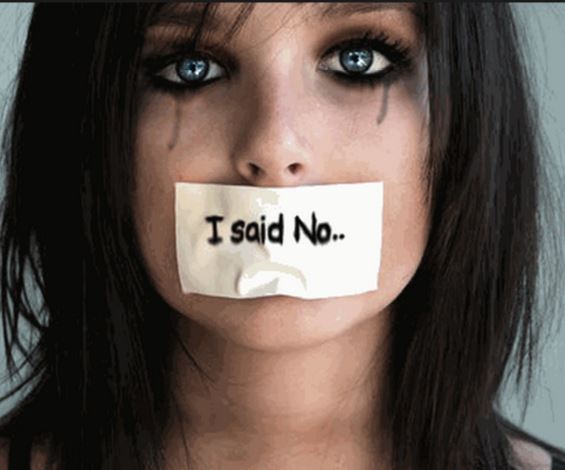 If you have not read the latest essay and editorial about scandalous physician behavior published in the Annals of Internal Medicine (AIM), you must do so now. They describe horrific racist and sexist remarks made about patients by senior male physicians in front of their young peers. The physicians-in-training are scarred by the experience, partially because the behavior itself was so disgusting, but also because they felt powerless to stop it.
If you have not read the latest essay and editorial about scandalous physician behavior published in the Annals of Internal Medicine (AIM), you must do so now. They describe horrific racist and sexist remarks made about patients by senior male physicians in front of their young peers. The physicians-in-training are scarred by the experience, partially because the behavior itself was so disgusting, but also because they felt powerless to stop it.
It is important for the medical community to come together over the sad reality that there are still some physicians and surgeons out there who are wildly inappropriate in their patient care. In my lifetime I have seen a noticeable decrease in misogyny and behaviors of the sort described in the Annals essay. I have written about racism in the Ob/Gyn arena on my blog previously (note that the perpetrators of those scandalous acts were women – so both genders are guilty). But there is one story that I always believed was too vile to tell. Not on this blog, and probably not anywhere. I will speak out now because the editors at AIM have opened the conversation.
When I was a third-year medical student I was assigned to tag along with an ophthalmology resident serving his first year of residency as an intern in general surgery. We were to cover the ER consult service one night, and our first patient was a young Hispanic girl with abdominal pain. It was suspected that she may have had appendicitis. Part of the physical exam required that we rule out a gynecologic cause of the pain. And so a pelvic exam was planned for this young girl of about 12 or 13. She was frightened and clinging to her grandmother. She had never seen a gynecologist before and had explained through her grandmother that she was a virgin – making a gynecologic cause of her abdominal pain less likely. I offered her some reassurance with my broken Spanish and held her hand as we wheeled her on a stretcher to a private examining room. The resident whispered in my ear, “This is going to be fun.”
The resident was creepy at every stage of the exam. He was clearly relishing the process, slowly instructing the poor girl to position herself correctly on the table. He held her knees apart as she whimpered and cried. He pretended to have difficulty positioning the speculum, inserting and reinserting it an unconscionable number of times. All-in-all it probably took ten minutes for him to get a cervical sample (this usually takes under 60 seconds). He performed the bi-manual portion of the exam in a bizarre, sexualized manner. I was furious and nauseated.
The patient was finally returned to her grandmother and the resident took me aside to ask how I thought he did. The perverted expression on his face was not lost on me. I looked at him with daggers in my eyes, but I knew that if I confronted him head-on it could trigger an investigation and in the end I had no hard evidence to prove that he had done anything wrong. It would wind up being a “he said, she said” scenario. I mustered the courage to say, “I think you were slow.”
For a fleeting moment he was taken aback by my insubordinate criticism and then he said the sentence that still haunts me today, “Well it was her first time.”
Each time I think of this interaction I feel sick to my stomach. I wonder what more I could have done.* I wonder if he is still out there violating his patients, and if anyone has ever confronted him. My only consolation, I suppose, is that he did not go on to become an Ob/Gyn. As an ophthalmologist one would hope that he had fewer opportunities for sexual abuse of patients.
I guess you could say that in my medical training, I witnessed a child rape. I don’t think it gets much worse than that… and I don’t know what to do with this horrific memory. I am forever changed.
It is my hope that these sorts of situations become true “never events” and that we create a protective environment where there are no career consequences for medical students thrust into the unfortunate position of whistle blower. Maybe the courageous AIM editorial is the first step towards redemption and healing.
*Note that I never saw this resident again. Our paths did not cross after the incident, and it was only at the end of the exam that I fully recognized the evil of his intent.
August 5th, 2015 by Dr. Val Jones in True Stories
No Comments »

A wrist graft similar to what my friend's husband required.
I watched helplessly as a dear friend went through the emotional meat grinder of a new cancer diagnosis. Her husband was found to have melanoma on a recent skin biopsy, and she knew that this was a dangerous disease. Because she is exceptionally intelligent and diligent, she set out to optimize his outcome with good information and the best care possible. Without much help from me, she located the finest specialists for her husband, and ultimately he received appropriate and state-of-the-art treatment. But along with his excellent care came substantial (and avoidable) emotional turmoil. The art of medicine was abandoned as the science marched on.
First came the pathology report, detailed and nuanced, but largely uninterpretable for the lay person. She received a copy of it at her request, but without any attempt at translation by her physician. In his view, she shouldn’t be looking at it at all, since it was up to him to decide next steps. She brought the report to me, wondering if I could make heads or tails out of it. Although I am not trained in pathology, I did know enough to be able to translate it, line-by-line, into normal speak. This was of great comfort to her as the ambiguity of prognosis (rather than certainty of metastasis and or mortality, etc.) was clearly outlined for the trained eye.
Then came the genetic testing and node biopsy. She was told that the tests could identify variants that would portend poorer outcomes, though it would take 6 weeks to find out if he had “the bad kind of melanoma.” Those 6 weeks were excruciating for her, as she planned out how they would manage financially if he needed treatment for metastatic disease, and if his life were shortened by various numbers of years. At week 6 they received no word from the physician, and so she called the office to inquire about how much longer it would take for the genetic testing to come back. She was rebuffed by office staff and was instructed to be patient because the lab was “processing an unusual number of samples” at this time.
Another week of anguish passed and she decided to contact the lab directly. As it turned out, they were eagerly awaiting the arrival of her husband’s sample, but it had been “lost” in hospital processing somehow. She called the hospital’s facility and someone found the tissue under a pile of other samples and tagged it appropriately and sent it on to the genetics lab. The hospital apologized for the delay via email – and she forwarded the note to her oncologist, so that he could sort out the potential processing bottleneck for other patients going forward.
The result was reported to the oncologist within a week’s time and in turn, the physician called (at 6:30am on a Monday morning) to discuss the result with my friend’s husband. He missed the call as he was in the shower getting ready for work, and wound up playing phone tag with the physician’s office for 3 more days. My friend had her heart in her mouth the entire time. She continued to imagine a world without her husband. If the disease stole him from her, how would she manage? What about the children? Could she make enough money alone to support her family?
“Why didn’t the physician leave any hint of the result in the phone message? If it was good news, surely he would have mentioned that.” She presumed. The physician required his patient to come into the office to discuss the results. And so they booked the next available time slot, another couple of days later. My friend was certain this was a bad sign.
As they arrived at the oncologist’s office, the staff forbade my friend to accompany her husband to the meeting. “Clinic policy” they stated. My friend’s mind was now spinning out of control – maybe my husband needs to be alone with the doctor because the results are so devastating that he must hear it by himself?
She insisted, nonetheless, to accompany him – and the staff felt obligated to clear it with the oncologist before they allowed her to enter the examining room with her husband. They whispered to him in another room before giving her the irritated nod that she could proceed. You could have cut the tension with a knife… she was certain that a death sentence was about to be handed down.
Once the oncologist entered the room, he spent the first 10 minutes making excuses for the delay in genetic tissue results. He argued that the hospital lab was actually not at fault for the delay and listed all the various reasons why nothing had been done incorrectly. His was so single-mindedly focused on the email he received weeks prior (simply describing the delay — as if it were some kind of assault on his own competency) that he almost left the room without telling them the results of the genetic test and biopsy sample.
As an afterthought at the end of the meeting, he announced: “Oh, and the tests suggest that you have a melanoma that is extremely unlikely to metastasize. The wide excisional biopsy is likely curative.”
And off he swished, white coat flowing behind him as he flung wide the door and moved on to the next patient.
The irony is that my friend’s husband got “great” medical care with a large helping of unnecessary suffering. His initial biopsy, wide excision and skin grafting, lymph node testing, and genetic lab studies were all appropriate and helpful in his diagnosis and treatment. But the way in which the information was presented (or not presented) was what made the entire process so painful. Unfortunately, we spend most of our time as physicians focused on the technicalities of what we do, rather than the emotional consequences they have on our patients and their families.
As we continue to “deliver healthcare” to our patients, let’s remember not to serve up any sides of unnecessary mental anguish. Clear and timely communication makes a world of difference in patient anxiety levels. And reducing those is part of the art of medicine that is so desperately needed, and disturbingly rare these days.
 I’m often asked to do book reviews on my blog, and I rarely agree to them. This is because it takes me a long time to read a book – and then if I don’t enjoy it, I figure the author would rather me remain silent than publish my true thoughts. Most of the reviews that I end up writing are unsolicited, but today is an unusual exception. A colleague asked me to read her book, “How To Be A Rock Star Doctor.” I got half way through when she checked in to see how things were going. I had to tell her that I didn’t agree with some of her advice to young doctors, and I worried that she would be discouraged by my honesty.
I’m often asked to do book reviews on my blog, and I rarely agree to them. This is because it takes me a long time to read a book – and then if I don’t enjoy it, I figure the author would rather me remain silent than publish my true thoughts. Most of the reviews that I end up writing are unsolicited, but today is an unusual exception. A colleague asked me to read her book, “How To Be A Rock Star Doctor.” I got half way through when she checked in to see how things were going. I had to tell her that I didn’t agree with some of her advice to young doctors, and I worried that she would be discouraged by my honesty.



 If you have not read the latest essay and
If you have not read the latest essay and 







