December 25th, 2011 by ChristopherChangMD in News, Opinion
No Comments »

 I admittedly snorted out loud when I read a New York Times article earlier last week regarding increased physician distraction due to electronic devices, especially with the advent of the smartphone with its emails, text messages, calls, and other alerts that ping intermittently throughout a typical work day.
I admittedly snorted out loud when I read a New York Times article earlier last week regarding increased physician distraction due to electronic devices, especially with the advent of the smartphone with its emails, text messages, calls, and other alerts that ping intermittently throughout a typical work day.
There is no question that electronic devices distract physicians as the article pointed out… But that’s like complaining about a leaky faucet when there’s a flooded basement and a hole in the roof.
The bigger problem that should be mentioned is hospital bureaucracy which probably creates just as much if not more unintended distractions for physicians and nurses.
What many patients and lay public may not realize is that Read more »
*This blog post was originally published at Fauquier ENT Blog*
December 14th, 2011 by GarySchwitzer in Opinion
1 Comment »


Some months I can’t wait for my new issue of Prevention magazine to arrive, just so I can see how they’ve stretched the envelope this time.
How about this month’s cover, trumpeting a Cancer Vaccine Breakthrough in big yellow font at lower left of the cover?
So I started flipping through the Table of Contents for the big story. Hmmm….nothing there. Odd.
So I started flipping through the pages of tips for “jiggle-proof arms and abs” and such and….voila…on page 13 I found the big story under another “Cancer Breakthrough” heading.
In 16 words in that little box, I learned that a vaccine was Read more »
*This blog post was originally published at Health News Review*
December 10th, 2011 by ChristopherChangMD in Medblogger Shout Outs, Research
3 Comments »

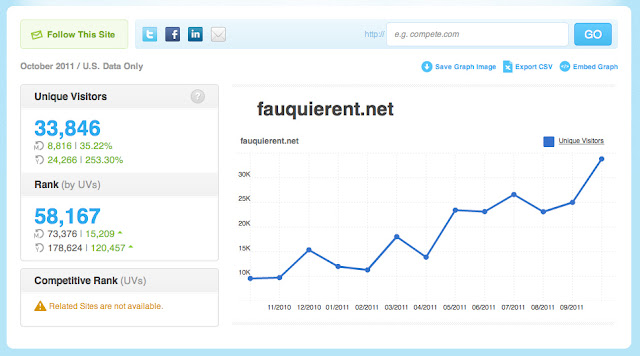
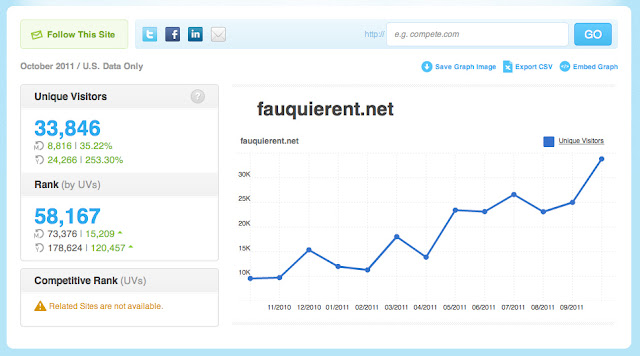
An interesting blog article from the folks at Compete came to my attention recently. Compete for those who don’t know is a fantastic analytics site to see how ANY website is doing in terms of popularity (number of visitors in a given time period). The basic data is free. For more in depth information, there’s a charge.
For example, for our practice’s website, here is the Compete data I pulled which is pretty accurate based on my own analytics information:
My nearest local competitor in terms of website popularity is the hospital, Fauquier Health System: Read more »
*This blog post was originally published at Fauquier ENT Blog*
November 9th, 2011 by Linda Burke-Galloway, M.D. in Better Health Network
No Comments »

 A recent article about the shameful infant mortality rate in the U.S. caught my attention. Certainly the statistics quoted are nothing new but still remains alarming. However, the Op Ed by CNN contributor Deborah Klein Walker gave the subject matter a new spin. Walker wrote “This is one of the greatest injustices in our country: that a baby’s chance of having a healthy life is largely dependent on where he or she is born. States and local communities vary widely in what care their leaders choose to provide to women and children.” If Dr. Walker were present, I’d give her a great big hug for her courage to say what no one else dared. A baby can die based on a hospital zip code.
A recent article about the shameful infant mortality rate in the U.S. caught my attention. Certainly the statistics quoted are nothing new but still remains alarming. However, the Op Ed by CNN contributor Deborah Klein Walker gave the subject matter a new spin. Walker wrote “This is one of the greatest injustices in our country: that a baby’s chance of having a healthy life is largely dependent on where he or she is born. States and local communities vary widely in what care their leaders choose to provide to women and children.” If Dr. Walker were present, I’d give her a great big hug for her courage to say what no one else dared. A baby can die based on a hospital zip code.
Every pregnant mother needs to take a mini course in hospital politics because they are directly affected. A hospital is no longer a place of healing. It is a business and at times, ruthless. I have witnessed a colleague forced out of business because she said no when a hospital wanted to buy her practice so they withdrew her admitting privileges instead. I recall bitter battles with my former employer because I would not encourage my patients to deliver at a hospital that was notorious for Read more »
*This blog post was originally published at Dr. Linda Burke-Galloway*
October 16th, 2011 by Linda Burke-Galloway, M.D. in True Stories
No Comments »

 The story of Tanya* is compelling. She was 24 weeks pregnant with her third child and the hospital was threatening to send her home. Two years ago, she faced similar circumstances and delivered a baby at 23 weeks. Luckily, the baby is now two years old but the one before that was not so lucky. Tanya presented to a local hospital during her first pregnancy because of complaints of abdominal pain. She was sent home because her contractions “weren’t regular.” Ten hours later, Tanya returned to the hospital because of a “nagging feeling that something was wrong” although her contractions were still not regular. Unfortunately, her cervix was dilated and the contractions could not be stopped. Her son was born alive but died one hour later because the hospital was not equipped to deal with premature newborns. Tanya’s second pregnancy was similar to her first because she developed premature contractions again, at 23 weeks. As with the first pregnancy, her contractions were not strong and regular so she was discharged home from the hospital with a monitor that was supposed to help. It didn’t. Read more »
The story of Tanya* is compelling. She was 24 weeks pregnant with her third child and the hospital was threatening to send her home. Two years ago, she faced similar circumstances and delivered a baby at 23 weeks. Luckily, the baby is now two years old but the one before that was not so lucky. Tanya presented to a local hospital during her first pregnancy because of complaints of abdominal pain. She was sent home because her contractions “weren’t regular.” Ten hours later, Tanya returned to the hospital because of a “nagging feeling that something was wrong” although her contractions were still not regular. Unfortunately, her cervix was dilated and the contractions could not be stopped. Her son was born alive but died one hour later because the hospital was not equipped to deal with premature newborns. Tanya’s second pregnancy was similar to her first because she developed premature contractions again, at 23 weeks. As with the first pregnancy, her contractions were not strong and regular so she was discharged home from the hospital with a monitor that was supposed to help. It didn’t. Read more »
*This blog post was originally published at Dr. Linda Burke-Galloway*
 I admittedly snorted out loud when I read a New York Times article earlier last week regarding increased physician distraction due to electronic devices, especially with the advent of the smartphone with its emails, text messages, calls, and other alerts that ping intermittently throughout a typical work day.
I admittedly snorted out loud when I read a New York Times article earlier last week regarding increased physician distraction due to electronic devices, especially with the advent of the smartphone with its emails, text messages, calls, and other alerts that ping intermittently throughout a typical work day.