September 15th, 2009 by KerriSparling in Better Health Network, Health Tips, True Stories
Tags: Bad Habits, insulin, Kerri, Six Until Me, Type 1 Diabetes
No Comments »

 Taking a cue from Rachel and Cherise, I wanted to post my diabetes “bad habits.” (Unfortunately, it didn’t take long to come up with six.) But thankfully, after months and months of extreme tweaking, my bad habits aren’t nearly as bad as they used to be.
Taking a cue from Rachel and Cherise, I wanted to post my diabetes “bad habits.” (Unfortunately, it didn’t take long to come up with six.) But thankfully, after months and months of extreme tweaking, my bad habits aren’t nearly as bad as they used to be.
1. Bolus-Stacking. (See also: rage bolusing) I have a very, very bad habit of stacking boluses when my blood sugar is high. You know … test and see that 212 mg/dl, take two units to correct it back to 100 … test again 45 minutes later to see 245 mg/dl staring back at you … freak out and take another unit for good measure … test one more time an hour later to see no real change … lace in two more units because you’re angry and frustrated and sick of the high … only to crash five hours later with a 45 mg/dl with your face mushed into a can of Pillsbury frosting. Not that I’ve done that. But if I were to do that, it might play out just like that.
2. Carb Winging It. Until recently, I’ve been an estimator. A SWAGger (scientific wild-ass guesser). Someone who kind of wings the whole carb-counting thing and hopes that there were only about 15 grapes in that snack bag or that the apple was really “small” instead of “medium.” With the little weeny doses of insulin I take, counting carbs with precision is crucial to making sure my numbers stay stable, so when I’m guessing as to the carb count, the blood sugar results go all over the place.
3. Shooting with a Mouthful. This is a bad habit pointing out by my endocrinologist a few months ago, and one that was wicked hard to break. And I have no idea how I ended up in this terrible habit to begin with, but it’s not good. I had a terrible tendency to start eating, then decide to bolus. Even if the carbs were counted perfectly and the insulin dose went in without issue, I wasn’t giving the insulin any time to act before introducing the carbs. Thus, making my numbers go berserk after meals. No more shooting while I’m eating. Now I need to shoot up before eating. Makes a big difference.
4. Self-Consious During Workouts. Another bad habit. When I go to the gym, I used to leave my insulin pump at home and then reconnect when I returned. It worked out to keep me from going low during workouts, yes, but it was also because I didn’t like having the device attached to me while I was wearing form-fitting workout clothes. Stupid Kerri. Sure, I was avoiding the lows, but I was also ending up close to 180 mg/dl by the end of my workout. With pre-pregnancy goals of 150 or lower, this is unacceptable. So I have to suck it up and wear the pump while I exercise and even sometimes go easier during a workout to avoid lows, instead of sacrificing blood sugar control for an extra mile on the treadmill.
5. Log Lagging. I have a good habit of starting logbooks, but a terrible time keeping up with them. This has been a hard habit to break (habit to break), but I’m close to turning it around. Logbooks are my diets – I am excellent at the outset, but then I fall apart. Thankfully, I’ve got a team at Joslin and a husband at home who are helping keep me accountable, and it’s making a world of difference.
6. Blame Game. And a sixth (but certainly not the last) bad diabetes habit that I have is my role in the blame game. I put a lot of pressure on myself to get things “right” and when the diabetes outcome isn’t what I’m hoping for, I tend to blame myself. I have to constantly remind myself that strong efforts and a decent attitude go a long way in this marathon, and I can’t beat myself up for every low or high that crops up randomly. Diabetes isn’t fair, and it isn’t easy, and it sure as hell isn’t my fault, so I just need to roll with the punches as gracefully as I can.
What are your diabetes bad habits? Or maybe it’s better to ask – what are your good diabetes habits? I’m going to have to concoct another “good” list soon – they’re way more fun. 🙂
*This blog post was originally published at Six Until Me.*
September 14th, 2009 by Dr. Val Jones in Announcements, Better Health Network, Expert Interviews, Health Policy, News, True Stories, Uncategorized
Tags: Cancer, Dead, Death, Died, Dirty Dancing, Hollywood, Oncology, Pancreas, Pancreatic Cancer, Patrick Swayze, Star
No Comments »
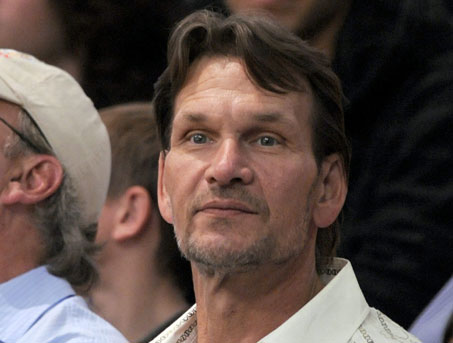
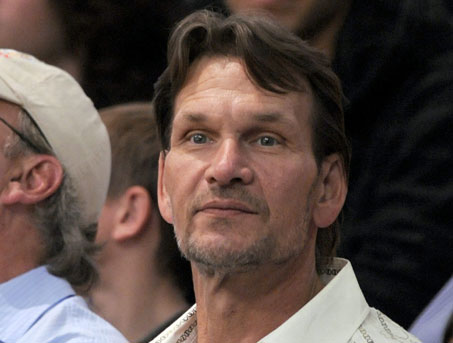 Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Pancreatic cancer is among the more deadly forms of cancer. I asked GI oncologist, Heinz-Josef Lenz, M.D., professor of medicine and professor of preventive medicine in the Division of Medical Oncology at the Keck School of Medicine at the University of Southern California, to explain why that’s so.
Dr. Val: Why is pancreatic cancer so much more deadly (i.e. less treatable) than many other forms of cancer?
Dr. Lenz: Unfortunately we don’t have very effective drugs for pancreatic cancer, which makes it one of the deadliest cancers of all. The median survival is about 8 months with metastatic disease. Even when the tumor is successfully removed there is a very high risk for tumor recurrence. We need more funding to better understand the risk for pancreatic cancer and identify and develop more effective therapies.
Dr. Val: Can you describe the typical course of metastatic pancreatic cancer?
Dr. Lenz: Unfortunately, the 5 year survival rate for pancreatic cancer is only 15 to 20%. The average survival after diagnosis is 12 to 19 months. The best predictor of long term survival is if the tumor is found and removed before it reaches 3 cm in size. Patients with metastatic pancreatic cancer are usually treated with a combination chemotherapy consisting of gemcitabine, tarceva, xeloda or oxaliplatin. However the response rates are (despite using aggressive combination therapies) low. Large clinical trials recently did not show any benefit from erbitux or avastin, again demonstrating that pancreatic cancer therapy is a difficult clinical challenge.
Dr. Val: Are certain populations at higher risk than others for pancreatic cancer?
Dr. Lenz: Age is the most important risk factor for this cancer. It is most common in individuals over age 50 and increases in frequency with age. Black men and women are slightly more likely to get pancreatic cancer (though the reasons for this are unclear), and men are slightly more likely than women to get the cancer. Other risk factors are smoking, diabetes, and obesity.
Dr. Val: If you suspect that someone is “high risk” for pancreatic cancer, what tests should he/she have?
Dr. Lenz: Patients with a genetic predisposition for breast cancer known as BRCA are also at higher risk for pancreatic cancer. There is also a familial form of pancreatic cancer. These high risk families are being followed up with specific screening plans. However there is not a reliable test for pancreatic cancer. Imaging with CT or MRI can miss pancreatic cancer and there is no reliable blood marker. The most common used is CA 19-9, which can be used for monitoring and diagnosis but is not elevated in all patients.
Dr. Val: What if the cancer is caught very early? Does that increase likelihood of survival?
Dr. Lenz: Absolutely. The best chance of survival is when the cancer is limited to the pancreas, and is surgically removed before it reaches a size of 3 centimeters. There are certainly people who have been cured this way, but unfortunately it’s very rare to catch the cancer at such an early stage since it usually has no symptoms until it’s quite advanced.
***
There is a wonderful advocacy group for those whose lives are touched by pancreatic cancer: PanCAN. One of PanCAN’s founders, Paula Kim, is a friend of mine and was inspired to create the organization after her dad was diagnosed with pancreatic cancer in 1999. At that time there was very little advocacy for this deadly disease. PanCAN helps people with pancreatic cancer find help and support.
September 14th, 2009 by Berci in Better Health Network, News
Tags: Memory, Memory Loss, Neurology, Psychiatry, Psychology, Twitter
No Comments »

At this year’s British Science Festival, Tracy Alloway, a psychologist from Stirling University, said the following:
Some examples of what can hurt or harm working memory include things like Twitter. When you’re receiving an endless stream of information when you’re a ‘tweeter’, it’s also very succinct, so there’s no need to process or manipulate that information, it’s not a dialogue unlike something like Facebook where you might be updating your status and so on.

Fortunately, Mark Henderson at Times Online puts things in the right place:
Most people I know who use Twitter see it as an interactive tool for conversing with wide groups, and for drawing like-minded people’s attention to information that might interest them. It’s interactive, full of links, and information-rich. It’s a misconception that the 140-character limit makes depth impossible. In fact, to me, Twitter seems to build social networks just as effectively as Facebook, which Alloway thinks might improve working memory.
Mark is right, and I have a few examples that can explain why I think so:
*This blog post was originally published at ScienceRoll*
September 14th, 2009 by Emergiblog in Better Health Network, Opinion
Tags: Census, Emergency Medicine, Hospital, Nursing, Predicting Volume, Shifts, Staffing
No Comments »

 Emergency has something in common with Labor & Delivery.
Emergency has something in common with Labor & Delivery.
Neither department has control over their census.
Medical/surgical, telemetry units and ICUs have a finite number of beds. When they are full, they are full; they cannot physically expand to more beds.
ED patients and laboring women are never turned away no matter how full the department may be. Oh, the ED may triage and L&D may send a patient in early labor home, but in both cases, eventually, all will be seen.
Labor and delivery has one advantage over the ED.
They can have someone on call.
I’ve never worked in an ED that has had an “on-call” nurse.
****
I will never understand the logic behind staffing an ED based on the previous 24 hour census.
If the ED does not meet a pre-determined number of patients on one day, the break nurse for the next day is canceled and there is much wailing and gnashing of teeth as the department goes over budget.
Never mind that the acuity level of the patients who were seen was through the roof. Or that 50% of them were admitted. Or that the next day, acuity again sky high, the nurses go without meals/breaks and the department is required to give penalty pay. Again, there is much wailing and gnashing of teeth for having to pay this penalty, a penalty that would never have been required had the break nurse not been canceled.
****
Now if the ED is slow, staff can always go home early. But not too early, because you never know what is coming in through the doors. So maybe an hour, 90 minutes early, knowing that the remaining staff can handle whatever they need to handle until the next shift comes in.
But what happens when the patients overwhelm the staff, both in acuity and numbers? Ambulance diversion doesn’t stop the walk-in critical patients. The MIs and the possible CVAs. The GI bleeders. The potentially septic. Trying to get patients out of the department and up to the floor doesn’t work when the floor won’t take the patient for four hours because it would put them “out of ratio”.
This is a huge issue on the night shift. When there is only one unit clerk/registrar, two nurses and an ED tech after 0300.
Of course, at night it is feast or famine.
Either the feces hits the proverbial fan or…it doesn’t.
Which is exactly why we need a nurse on-call.
The ED needs flexible staffing that accounts for those times when the acuity level/census is overwhelming. Not canceling the extra break nurse is one way of doing that on days and evenings; using the on-call system is another way that could be utilized at night. If it can be done in L&D, why can’t it be done in the ED? Surely the money saved in penalty pay for missed breaks and meals would make it budget neutral.
All I know is that trying to drop staff in an ED based on what happened the previous 24 hours makes zero sense.
(And don’t even get me started on why nurse-patient ratios are treated like unbreakable rules on the floors, but it’s okay for the ED to be waaaaay out of ratio and nobody blinks….that’s another whole post!)
*This blog post was originally published at Emergiblog*
September 14th, 2009 by EvanFalchukJD in Better Health Network, Opinion
Tags: Congress, Health Insurance, Healthcare reform, Obama, Public Plan, Reactions, Reform, Speech
No Comments »

Eight quick reactions to the President’s speech:
1. It was a good speech. Reaction around the blogosphere and elsewhere seems to be dependent on how you felt about reform plans going in. If you were in favor, you thought it was terrific (warning strong language at the link); if you were against, you thought it was disingenuous.
2. The interesting question is how people who weren’t sure will react. By this I mean people who are anxious that reform will affect their health care in ways they don’t like. There is still the mixed message that created this anxiety in the first place. On the one hand, the President repeated “Nothing in this plan will require you to change what you have. “ Sounds like no big deal. On the other hand, he quoted Ted Kennedy as saying the plan “is above all a moral issue; at stake are not just the details of policy, but fundamental principles of social justice and the character of our country.” Sounds like a very big deal. Which is it?
3. The boorish Congressman who screamed “you lie!” at Obama during the address must have been confused and thought he was at a town hall meeting. But I’ve always thought it would be cool if we had a “Question Time” like they do in the UK. Presidents would have to face much more interesting and uncomfortable questions than they otherwise get, and it would make for a terrific spectacle. Obviously this wasn’t the time or place for that sort of thing. And if we ever do get an American Question Time, representatives will have to come up with better questions than “you lie,” too.
4. The President talked about “30 million American citizens who cannot get coverage.” This is different from the 46 million “uninsured” he usually talks about. The Associated Press thinks the other 16 million are people who could buy or otherwise get coverage but choose not to, as compared to those who want coverage but can’t afford it.
5. I was surprised to hear the President give more than just a nod to the Facebook health care status update meme. I mean he quoted it directly: “in the United States of America, no one should go broke because they get sick.” This must be the first time a President has ever quoted something from Facebook in an address to Congress – it’s some kind of a milestone for social media. Thoughts on that meme are here.
6. The President talked about the uncompetitive insurance market, noting that “in 34 states, 75 percent of the insurance market is controlled by five or fewer companies.” It sounds like he’s not just talking about the “public option” when he talks about creating competition in these markets. His idea of insurance exchanges and a federal health insurance regulator seem to be direct challenges to the state-by-state system of insurance regulation. It will be interesting to see the reaction of state insurance regulators to this speech.
7. I was right: the President didn’t talk about the three things I said he wouldn’t talk about. In fact, he said almost nothing about the delivery of care- it was all about how to pay for it.
8. The President got some laughs with his comment that he thinks “there remain some significant details to be ironed out.” He’s right, and there’s the rub. Whether and how that ironing out happens was the question before the President’s speech, and it’s still the question today.

*This blog post was originally published at See First Blog*
 Taking a cue from Rachel and Cherise, I wanted to post my diabetes “bad habits.” (Unfortunately, it didn’t take long to come up with six.) But thankfully, after months and months of extreme tweaking, my bad habits aren’t nearly as bad as they used to be.
Taking a cue from Rachel and Cherise, I wanted to post my diabetes “bad habits.” (Unfortunately, it didn’t take long to come up with six.) But thankfully, after months and months of extreme tweaking, my bad habits aren’t nearly as bad as they used to be.





 Emergency has something in common with Labor & Delivery.
Emergency has something in common with Labor & Delivery.








