December 11th, 2012 by Dr. Val Jones in Health Tips
No Comments »
 I’ve continued to have terrific email questions and answers with the Boys & Girls Clubs’ Fit Family Challenge participants. I thought I’d publish some of our conversations so that you can participate as well. The Lang family shared this image of their son eating dinner next to the latest USDA dietary recommendations “MyPlate” materials. A picture’s worth 1000 words, isn’t it?
I’ve continued to have terrific email questions and answers with the Boys & Girls Clubs’ Fit Family Challenge participants. I thought I’d publish some of our conversations so that you can participate as well. The Lang family shared this image of their son eating dinner next to the latest USDA dietary recommendations “MyPlate” materials. A picture’s worth 1000 words, isn’t it?
This cute fella is a healthy weight, he is very athletic, and he’s also wondering where chicken nuggets, french fries, and pizza fit in to the MyPlate dinner plans… His mom asked me how to make more “kid friendly” healthy meals. Perhaps some folks reading this have some success stories that they’d like to share? Here’s what I had to say to the Langs and others…
1. My son doesn’t think the MyPlate suggested meals are kid friendly. What can we do?
I wonder if your son would be open to trying healthier variations of the foods he likes? You could make a pretty tasty pizza with whole wheat crust, grilled veggies, a little pesto or tomato sauce and some ham cubes (ham is much lower in fat than sausage or pepperoni) and low fat shredded mozzarella. You can get a pizza stone to help crisp the crust in a regular oven. The pizza would probably reheat well so you could make it in advance too.You can bread chicken strips and bake them (instead of frying them) to simulate healthy chicken “nuggets.” Same for fish sticks. You can try sweet potato fries for a healthier fry option – bake them in the oven with a little olive oil, salt and pepper. More nutritious, kid-friendly recipes may be found at KidsHealth.org
2. Do my kids need 8 cups of water a day?
As far as water is concerned, the amount you need really depends on how much liquid you’re getting from other sources (food, beverages) as well as how much you’re sweating (exercise), how hot/dry the environment is and how much you weigh. Eight cups/day is a very rough rule of thumb. Some people need more or less depending on the day. Unless you are doing extreme exercise (in the heat) that requires fluid replacement before you notice that you’re thirsty, thirst is a good indicator of whether or not you need to drink. Also, I’ll tell you a doctor secret – all you need to know about hydration is in your urine color. Urine becomes very concentrated (dark yellow) when you are dehydrated. If you drink enough water to keep your urine a nice light yellow, then that’s all you need.
3. What are the best vegan protein substitutes for meat?
Concentrated vegetable protein is primarily derived from soy (tofu and tempeh) and wheat (seitan). Nuts and seeds also contain some degree of protein, as well as beans, lentils, and rice. Tofu, tempeh, and seitan can be molded into burger and hotdog shapes and may be prepared to mimic meat flavors. Keep in mind that concentrated soy or wheat proteins may not agree with your intestinal tract (some complain of excessive gas and bloating). So if you have those reactions, at least you’ll know that it’s quite common.
4. Is it healthy to be a vegetarian? Is there such a thing as too much fruit and veggies?
Vegetarianism can be healthy, though it takes some effort to ensure that adequate amounts of nutrients are received – especially if you’re vegan (no dairy, no eggs). The most common deficiencies for vegans are iron, B12, calcium, Omega-3 fatty acids, protein, and Vitamin D. (You can read more about how vegetarians can overcome these deficiencies here.) I guess my main concern with veganism is the low omega-3s. It is basically impossible to get enough omega-3 fatty acids from plant sources (certain seeds, you may have heard, have a good amount of omega-3 fatty acids but what they won’t tell you is that plant omega-3’s aren’t processed by the body so they remain inactive and don’t provide much benefit.) Omega 3 fatty acids form a protective layer on the outside of cell membranes by reducing inflammation. This is particularly helpful in the reduction of plaque build up in heart arteries, and reducing the risk of various dementias (such as Alzheimer’s) that have an inflammatory cause.
Excellent sources of omega 3 fatty acids are oily fish (sardines, salmon, mackerel, sea bass). This is why the American Heart Association (and MyPlate.gov) recommend 2 servings of oily fish/week for optimal health. Vegetarians are missing out on this important benefit.
As far as eating too many fruits/veggies is concerned – I can’t think of too many potential harms from eating large amounts of fruits/veggies (other than weight gain if you really eat a lot of fruit – they have quite a bit of natural sugar). The real harm comes from excluding vital nutrients by eating plants exclusively (without a careful strategy to get the right plant sources of vitamins and minerals, along with omega-3 supplements).
December 7th, 2012 by Dr. Val Jones in Health Tips
No Comments »
 This year’s Fit Family Challenge competitors are smart, savvy, and full of great nutrition-related questions! I just finished a one hour conference call with 10 family finalists from across the U.S. and Hawaii. As part of their challenge to adopt healthy diet and exercise practices, they were asked to send me their most burning nutrition questions. One mom told me that her goal was “to teach her girls how to think critically” about health information. I was so pleased to see those values being promoted that I thought I’d share some of our mythbusting FAQs here on the blog:
This year’s Fit Family Challenge competitors are smart, savvy, and full of great nutrition-related questions! I just finished a one hour conference call with 10 family finalists from across the U.S. and Hawaii. As part of their challenge to adopt healthy diet and exercise practices, they were asked to send me their most burning nutrition questions. One mom told me that her goal was “to teach her girls how to think critically” about health information. I was so pleased to see those values being promoted that I thought I’d share some of our mythbusting FAQs here on the blog:
1. I live in a community that doesn’t add fluoride to the public water supply. Do my kids need to take fluoride supplements?
Fluoridation of our water supply is considered to be one of the top 10 most effective public health initiatives of the 20th century. Enhancing the natural fluoride content of water results in up to a 60% reduction in tooth decay for kids! The cost to a community of adding fluoride to the water supply is about 50 cents per person per year, so it’s really quite affordable. I’m not sure why your community water hasn’t been fluoridated, but it’s estimated that about 1/3 of Americans still live in communities that haven’t supplemented their water with fluoride (so you’re not alone).
Our teeth use fluoride to strengthen our enamel – and we can get fluoride to our teeth in two ways: 1) from our blood stream (e.g from the water we drink, digest, and absorb) and 2) topically (e.g. from toothpaste). Studies have shown that it’s best to get fluoride via both routes for optimal enamel strength. For children living in areas where the water is not fluoridated, the American Dental Association (ADA) recommends fluoride vitamins until at least age 16. There are two strengths of fluoride vitamins, and the dosage required depends on the fluoride levels in the local water supply (you can ask your local Water Department for that information if you haven’t already). Keep in mind that most children’s permanent teeth (with the exception of “wisdom teeth”) erupt by age 13 – and before that age there is no way to get fluoride to them except via the blood stream. So digesting fluoride (via water or vitamins) is critical to strengthen those teeth that haven’t broken through the gums yet.
For more information about fluoride, see this helpful ADA guide.
2. Should parents be concerned about hormone levels in milk? Is there an advantage to buying organic milk?
All mammals release trace amounts of hormones into their milk. Cow’s milk naturally contains a small amount of bovine somatotropin (bST) which is a protein that is quickly broken down by our stomachs when we drink milk. Some farmers give their cows additional amounts of the hormone to stimulate milk production. This rbST (or BGH) is virtually identical to naturally occurring cow hormones and the decades of research we’ve collected has been reviewed by the FDA (Food and Drug Association), WHO (World Health Organization), NIH (National Institutes of Health), AMA (American Medical Association), and ADA (American Dietetic Organization) – and all agree that rbST is safe for human consumption in the levels it occurs in cow’s milk. Interestingly, studies have shown that milk hormone levels in organic milk is essentially identical to levels in regular milk. There is therefore no advantage in buying organic milk insofar as hormones are concerned.
I believe that cow’s milk is safe and nutritious for kids (so long as they have no milk allergies or lactose intolerances). The milk/hormone scare is kind of an urban legend, so I wouldn’t be too worried about it. Your girls haven’t suffered any harm from drinking regular milk – and it’s great that you all enjoy the skim variety, by the way. Lower calorie options can help you maintain your weight over your lifetime.
For more information about milk and hormones please check out this helpful link full of research resources.
3. Are there lifestyle choices that I can make to reduce my risk of getting cancer? Can vitamins help?
You are right that there are lifestyle choices that can substantially reduce your risk (and your childrens’ risk) of getting cancer. However, there is no way to guarantee that you’ll never get cancer, no matter how carefully you control your diet and lifestyle. Nevertheless it’s an excellent idea to do what we can to reduce our risks. Cancer is actually a complicated collection of different diseases, and so specific behavior changes may reduce the risk of certain cancers but not others. For example, a high fiber diet may reduce the risk of colon cancer, but not skin cancer.
Also note that it’s very hard to prove that any one dietary change (such as consuming a larger amount of one particular vitamin or herb) has a direct impact on cancer risk. What works is sometimes more general (such as avoiding becoming obese). Here are some behavior changes that have been scientifically proven to reduce cancer risks or prevent certain cancers:
1. Smoking cessation
2. Regular use of sunscreen
3. A diet rich in fiber (i.e.lots of fruits and veggies and whole grains)
4. Maintaining a healthy weight
5. Regular exercise
6. HPV vaccines (especially for young girls – can prevent cervical cancer) and hepatitis vaccines (can prevent liver cancer)
7. Drinking very little alcohol (no more than 1 drink/day)
Screening for cancer is also important – because catching a cancer early is often the best way to cure it. The most effective screening tests are:
1. Colonoscopies (for adults over age 50)
2. PAP smears (for sexually active women and women who haven’t had hysterectomies)
3. Physical exams to check for skin cancer, oral cancer, and testicular cancers
Mammograms and prostate blood tests are less effective at catching cancers early, but they are recommended by most medical professional associations.
I recommend reading this page at the National Cancer Institute for more information about avoiding cancer risk factors:
Multivitamins are not recommended for cancer prevention. Although it would seem that vitamins could help reduce the risk of cancer, large studies have shown that they do not reduce the risk of cancer, and may even increase one’s risk (especially vitamin E.) The best source of vitamins is healthy food – and their fiber benefits are excellent as well. For a nice summary of the unhelpfulness of vitamin supplements, please see this ABC News summary of recent research.
December 4th, 2012 by admin in Health Tips, Humor, Research
No Comments »
 In my last post I told you that I would reveal the one thing you can do to have a significant, positive and lasting effect on your brain health as you get older. See if you can spot it in the following list:
In my last post I told you that I would reveal the one thing you can do to have a significant, positive and lasting effect on your brain health as you get older. See if you can spot it in the following list:
a) Learn to dance Gangnam style
b) Join a choir
c) Catch a wave
d) Pump some iron
Ok, that was a trick question. All of these answers are somewhat correct, but I was looking for the “most” correct answer (flashbacks to undergrad, anyone?): Pump some iron.
I realize I sound like a broken record – I’ve already written about how aerobic exercise can promote healthy aging here and here, and I’ve even already written about resistance training, or lifting weights, here.
So why am I at it again? Because it’s important!
I’m fresh out of the 2012 Aging and Society Conference, where researchers came together to discuss what works and what doesn’t when it comes to healthy aging. It turns out everyone pretty much agrees that exercise is hands down the most effective intervention to keep your brain cells happy into old(er) age. All sorts of different types of exercise, ranging from simply walking to attending resistance training classes, are associated with different types of improvements in cognition, memory, and even brain size.
Of course, there are different levels of effort involved with different types of exercise, or even when talking about a single form of exercise. When my friend Jess asks me to go for a walk, she means a power walk: it usually involves going up hills, sweating like a pig (even though pigs, ironically, don’t sweat much), and barely having enough breath for girl talk (though somehow we always seem to find it). When my friend Al and I go for a walk, what he means is a “mosey”: we stop to look at the view, pet the dog, chit chat with strangers, and have more than enough breath for lengthy discussions about life, work, and the possibility of alien lifeforms. When it comes to brain health, whether you’re walking or pumping iron, a little sweating and effort can go a long way. For example, resistance training has been proven to be most effective when the load, or how much weight you are working with, increases over time. So kick the intensity up a notch: there will still be plenty of time for chit chat around a post-exercise, antioxidant-rich mug of matcha (my new obsession – stay tuned).
Now that the obvious has been (re)stated, I want to take this opportunity to discuss the idea that perhaps lifestyle interventions such as exercise could be prescribed by your doctor. We know that exercise can improve cognition in aging but also conditions like depression. Should physicians prescribe lifestyle changes? Or are diet, exercise, and other lifestyle activities choices we should make ourselves? How would you feel if your doctor prescribed you exercise instead of pills? Would you be more motivated to exercise if the prescription came from your doctor instead of from your friendly Internet science blogger? Your thoughts in the comments!
***
Dr. Julie Robillard is a neuroscientist, neuroethicist and science writer. You can find her blog at scientificchick.com.
November 30th, 2012 by Dr. Val Jones in Book Reviews
No Comments »
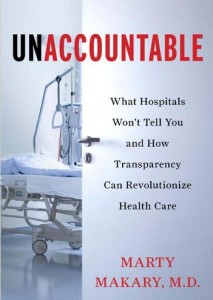 I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.
I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.
Just two months ago my fiancé sent me a “must read” article from the Wall Street Journal. It was Marty’s provocative piece, “How To Stop Hospitals From Killing Us.” The article was an excellent primer for his book, “Unaccountable: What Hospitals Won’t Tell You And How Transparency Can Revolutionize Health Care” which I highly recommend (holiday gifts, anyone?)
Unaccountable is both horrifying and oddly optimistic. Marty describes case after case of medical errors, lapses in judgment, and near misses in the surgical suite. He exposes the cultural foibles of the medical and hospital hierarchy, leaving no dirty stone unturned. Surgical delinquents such as Dr. Hodad (“hands-of-death-and-destruction”) are presented with detached accuracy, along with a clear list of reasons why the system fails to prevent the Hodads of the world from operating.
From the micro (individual physician mistakes) to the macro (trends in hospital safety breakdowns), Marty turns to survey data to make sense of the shortcomings. Interestingly, hospital “culture” (rated by its own employees) is the most predictive of overall hospital safety performance. Detailed record keeping of surgical complication rates correlates strongly with how employees rate their hospital on three simple questions:
1. Would you have your operation at the hospital in which you work?
2. Do you feel comfortable speaking up when you have a safety concern?
3. Does the teamwork here promote doing what’s right for the patient?
Marty’s conclusion that culture is the defining factor in patient safety and satisfaction ratings is both accurate and squishy. It’s difficult to create a reproducible template for a healthy work culture, and yet good culture is the basis for the success of hospitals such as the Mayo Clinic. Individual hospitals, like individual surgeons, have different personalities and temperaments. Raising them to be upstanding citizens involves a combination of good parenting and good luck.
Because I think Marty is absolutely right about culture as the foundation for safe and effective care, I think he’s also overly optimistic about the potential success of strategies to reproduce caring hospital cultures. By his own admission, not even the Mayo Clinic “mother ship” in Rochester, MN, has been able to create the exact level of quality care in its sister hospitals in Scottsdale, AZ, and Jacksonville, FL. So how can we dramatically improve patient care on a national level? Marty suggests that we need to find ways to force hospitals to become more transparent in order to revolutionize healthcare. His ideas include:
1. Mandatory hospital public reporting of patient re-admissions, complication rates, and never events.
2. Adoption of check lists by surgical teams to reduce errors.
3. Installation of video cameras throughout hospital floors and surgical suites so that staff behaviors can be monitored more effectively (e.g. to enforce hand washing or identify surgeons who have high error rates).
4. Accessible and transferable medical records that put patients at the center of their documentation.
While these ideas have merit, I believe they will fall short of achieving our ultimate goals. In my view, a culture of accountability is not the same as a culture of caring. Adopting certain “Big Brother” (cf. #3 above) strategies to pressure staff to behave/perform appropriately is only going to force the Hodads underground. We need staff to genuinely care enough about their patients to gang up on the Hodads and kick them out of the hospital for good. Caring doesn’t happen at a national level, it is personal and local. That’s why individual hospitals must develop their unique cultures for themselves, with progress measured by responses to those staff questions about whether or not they’d want to be cared for at their own institution.
I agree with Marty that hospital data transparency might be the best antiseptic we have to scrub the underbelly of medicine, though the ultimate success of our procedures will always be culture and surgeon-dependent. And that’s something you can’t regulate from Washington.
***
Marty’s book is available for purchase at Amazon.com.
Check out your local hospital safety scores from LeapFrogGroup.
November 28th, 2012 by Dr. Val Jones in Health Policy, Opinion, Primary Care Wednesdays
No Comments »
 Animal research has shown that the best way to get a rat to press a pellet-producing lever is to set the mechanism so that it doesn’t always release a pellet with each push. The unpredictability (or scarcity) of the reward causes the rat to seek it with more fervor. Casino owners are well aware of this phenomenon, gaming our brain’s natural wiring so that our occasional wins drive us to lose more than we would if our winning had a predictable pattern.
Animal research has shown that the best way to get a rat to press a pellet-producing lever is to set the mechanism so that it doesn’t always release a pellet with each push. The unpredictability (or scarcity) of the reward causes the rat to seek it with more fervor. Casino owners are well aware of this phenomenon, gaming our brain’s natural wiring so that our occasional wins drive us to lose more than we would if our winning had a predictable pattern.
I believe that the same principle is at work in physician reimbursement. Although most patients don’t realize this, physicians aren’t always paid for the work they do, and they are paid wildly different rates depending on how they code an encounter or procedure. After several health insurance denials of payment for legitimate work, physicians look for ways to offset their losses. Those may include changing the coding of their procedures to enhance the rate of reimbursement, exaggerating the complexity of an encounter, or (less commonly) billing for things they didn’t do. Because of the perceived injustice in a system that randomly denies payment for legitimate work, the physician feels less morally concerned about her over billing and coding foibles.
And so a vicious cycle of reimbursement deprivation, followed by fraud and abuse, becomes the norm in the U.S. healthcare system. Payers say that physicians are greedy and unethical, and physicians say that payers deny reimbursement unfairly and pay rates that are too low to be sustainable. The government’s response is to hire a cadre of auditors to ferret out physician fraud while cutting reimbursement to physicians further. This is similar to reducing the rate of pellet release to the rats in the Skinner boxes, while randomly electrocuting them through the metal flooring. The result will be that rats will work harder to find work-arounds to get their pellets, including gathering together into larger groups to share pellets. This is occurring more and more commonly as solo practitioners are joining hospitals or large group practices to make ends meet.
But we need to realize a few things about the “Skinner box healthcare system:”
1. Rats are not evil because they press levers manically when there is a scarcity of pellets. Physicians are not evil when they look for ways to make up lost revenue. While fraud and abuse are always wrong, it is not surprising that they are flourishing in an environment of decreasing reimbursement and increasing health insurance payment denials. If we want to address fraud and abuse, we need to understand why it’s happening so that our “solutions” (i.e. hiring thousands more government auditors to investigate medical practices) don’t end up being as useless as shocking the rats.
2. Health insurance (whether public or private) is not evil for trying to rein in costs. Payers are in the unenviable position of having to say “no” to certain expenditures, especially if they are of marginal benefit. With rats pressing levers at faster and faster rates for smaller and smaller pellets, all manner of cost containment mechanisms are being applied. Unfortunately they are instituted randomly and in covert manners (such as coding tricks and bureaucratic red tape) which makes the rats all the more manic. Not to mention that expensive technology is advancing at a dizzying rate, and direct-to-consumer advertising drives demand for the latest and greatest robot procedure or biotech drug. Costs are skyrocketing for a number of good and bad reasons.
3. There is a way out of the Skinner box for those primary care physicians brave enough to venture out. Insurance-free practices instantly remove one’s dietary reliance on pellets, therefore eliminating the whole lever pressing game. I joined such a practice several years ago. As I have argued many times before, buying health insurance for primary care needs is like buying car insurance for your windshield wipers. It’s overkill. Paying cash for your primary care allows you to save money on monthly insurance premiums (high deductible plans cost much less per month) and frees up your physician to care for you anywhere, anytime. There is no need to go to the doctor’s office just so that they can justify billing your insurance. Pay them for their time instead (whether by phone, in-person, or at your home/place of business) and you’ll be amazed at the convenience and efficiency derived from cutting out the middle men!
Conclusion: The solution to primary care woes is to think outside the box. Patient demand is the only limiting factor in the growth of the direct-pay market. Patients need to realize that they are not limited to seeing “only the physicians on their health insurance list” – there is another world out there where doctors make house calls, solve your problems on the phone, and can take care of you via Skype anywhere in the world. Patients have the power to set physicians free from their crazy pellet-oriented existence by paying cash for their health basics while purchasing a less expensive health insurance plan to cover catastrophic events. Saving primary care physicians from dependency on the insurance model is the surest path to quality, affordable healthcare for the majority of Americans. Will you join the movement?
 I’ve continued to have terrific email questions and answers with the Boys & Girls Clubs’ Fit Family Challenge participants. I thought I’d publish some of our conversations so that you can participate as well. The Lang family shared this image of their son eating dinner next to the latest USDA dietary recommendations “MyPlate” materials. A picture’s worth 1000 words, isn’t it?
I’ve continued to have terrific email questions and answers with the Boys & Girls Clubs’ Fit Family Challenge participants. I thought I’d publish some of our conversations so that you can participate as well. The Lang family shared this image of their son eating dinner next to the latest USDA dietary recommendations “MyPlate” materials. A picture’s worth 1000 words, isn’t it?

 This year’s
This year’s In my
In my 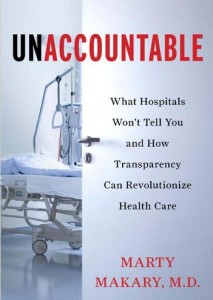 I met Dr. Marty Makary over lunch at
I met Dr. Marty Makary over lunch at