October 3rd, 2009 by David Kroll, Ph.D. in Better Health Network, Expert Interviews
No Comments »

 This morning, I once again get to join in with a group of noted journalists, authors, educators, and all-around people-who-do-things-I-can’t for the annual advisory board meeting of the M.S. in Medical and Science Journalism Program at the University of North Carolina at Chapel Hill’s School of Journalism and Mass Communication.
This morning, I once again get to join in with a group of noted journalists, authors, educators, and all-around people-who-do-things-I-can’t for the annual advisory board meeting of the M.S. in Medical and Science Journalism Program at the University of North Carolina at Chapel Hill’s School of Journalism and Mass Communication.
Program founder and current director, Tom Linden, MD, is a Yale- and UCSF-trained physician-journalist with extensive broadcast experience across a series of California television stations. Dr Linden also recognized very early the potential value and pitfalls of the web for communicating health information and published in 1995, with Michelle Kienholz, one of the first consumer guides to medical information on the internet. I also featured Tom here in December 2007 when he launched his own blog.
So today, Dr Linden has asked me to speak to about science and medical blogging but with respect to how it has augmented my own professional career. Read more »
*This blog post was originally published at Terra Sigillata*
October 1st, 2009 by Medgadget in Better Health Network, News
No Comments »


An international team of collaborators from a number of academic institutions and a couple pharmaceutical firms has been working with researchers at the National Institute of Standards and Technology (NIST) to study how special sugar coated iron oxide nanoparticles interact with each other to destroy cancer cells under laboratory conditions. The 100 nanometer wide particles, which are attracted by tumor cells, are particularly prone to magnetically induced heating.
Read more »
*This blog post was originally published at Medgadget*
September 24th, 2009 by Dr. Val Jones in Audio, News
No Comments »

Rudy Tanzi, Joe Perry, Francis Collins
I know. I was just as surprised as you are. Dr. Francis Collins, former director of the Human Genome Project, author of The Language Of God, and new director of the National Institutes of Health performed live in front of a group of Washington locals at the Capitol building today. He actually jammed with Aerosmith’s Joe Perry in an “unplugged” performance of Bob Dylan’s, “The Times They Are A Changin’.” This is not the kind of thing one expects in the hallowed halls of the Capitol building. But maybe it’s time to expect the unexpected?
I happened to have my reporter’s microphone with me in the audience so I recorded the song. The vocalist is Dr. Collins, Joe Perry does a guitar solo near the end, and Dr. Rudy Tanzi is on harmonica. The sound quality is… well… it’s what you’d expect from a hand-held microphone. But it’s worth a listen, just to get to know our new NIH director a little better!
[Audio:https://www.getbetterhealth.com/wp-content/uploads/2009/09/francis-collins.mp3]

Delta Goodrem
Australian pop star and cancer survivor Delta Goodrem followed Dr. Collins with this acapella beauty (again, forgive the sound quality):
[Audio:https://www.getbetterhealth.com/wp-content/uploads/2009/09/delta-goodrem.mp3]
A few things struck me about the event. First of all, Francis Collins is more of a “firecracker” than I expected. I read and reviewed his book recently, and his vivacious personality did not come through in its pages as well as it did on the stage with Joe Perry. He’s a fun-loving guy, a serious scientist, and very committed to advancing research and encouraging young people to rekindle their interest in discovery. That’s all very good news for America.
Secondly, I was touched by Joe Perry’s story about wanting to be a marine biologist when he grew up. Apparently he had a learning disability of some sort that was not addressed in school. For that reason, his test scores suffered and he looked for ways to excel outside of the classroom. His bright mind discovered an immediate affinity for music, and he poured himself into a career as a rocker. He still yearns for the ocean, though, and is a certified diver. As I looked at Joe, I kept thinking – my gosh, he might have been the next Jacques Cousteau if he had more help in school. But brilliance finds its own way to flourish – and Aerosmith became his outlet instead.
Thirdly, I realized that there are in fact a few congressmen with their heads screwed on straight when it comes to science. I had almost lost hope after watching video footage of Tom Harkin instructing scientists to validate his opinions rather than test whether or not certain things were true. Yikes. But the three co-chairs of the congressional biomedical research caucus, Reps Brian Bilbray, Mike Castle, and Rush Holt, seemed to truly understand some of the issues facing the advancement of medical research – and are determined to move America forward.
And finally, I noted that there wasn’t a single female or minority “rock star scientist” in the program. That made me a little bit sad. Are we really that rare? I guess we still have a long way to go on that front… And since Dr. Collins mentioned that only 15% of US students are enrolled in science or engineering bachelors’ programs (compare that to 50% in China or 75% in India) we are soon going to be playing catch up with the rest of the world in terms of scientific discovery.
So we’ve got our work cut out for us folks – with our youth’s waning interest in science education, the excessive red tape that is slowing down the process of producing cures, and the public getting their medical advice from the likes of Jenny McCarthy, there has never been a more important time to restore science to its rightful place.
Maybe Francis Collins is going to “bring sexy back” to science?
Whatever works!
***
More info on the Rock Stars Of Science program.
September 14th, 2009 by Dr. Val Jones in Announcements, Better Health Network, Expert Interviews, Health Policy, News, True Stories, Uncategorized
No Comments »
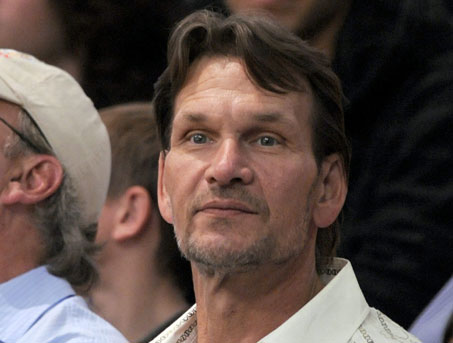
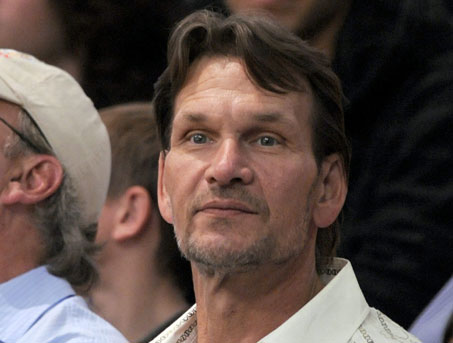 Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Pancreatic cancer is among the more deadly forms of cancer. I asked GI oncologist, Heinz-Josef Lenz, M.D., professor of medicine and professor of preventive medicine in the Division of Medical Oncology at the Keck School of Medicine at the University of Southern California, to explain why that’s so.
Dr. Val: Why is pancreatic cancer so much more deadly (i.e. less treatable) than many other forms of cancer?
Dr. Lenz: Unfortunately we don’t have very effective drugs for pancreatic cancer, which makes it one of the deadliest cancers of all. The median survival is about 8 months with metastatic disease. Even when the tumor is successfully removed there is a very high risk for tumor recurrence. We need more funding to better understand the risk for pancreatic cancer and identify and develop more effective therapies.
Dr. Val: Can you describe the typical course of metastatic pancreatic cancer?
Dr. Lenz: Unfortunately, the 5 year survival rate for pancreatic cancer is only 15 to 20%. The average survival after diagnosis is 12 to 19 months. The best predictor of long term survival is if the tumor is found and removed before it reaches 3 cm in size. Patients with metastatic pancreatic cancer are usually treated with a combination chemotherapy consisting of gemcitabine, tarceva, xeloda or oxaliplatin. However the response rates are (despite using aggressive combination therapies) low. Large clinical trials recently did not show any benefit from erbitux or avastin, again demonstrating that pancreatic cancer therapy is a difficult clinical challenge.
Dr. Val: Are certain populations at higher risk than others for pancreatic cancer?
Dr. Lenz: Age is the most important risk factor for this cancer. It is most common in individuals over age 50 and increases in frequency with age. Black men and women are slightly more likely to get pancreatic cancer (though the reasons for this are unclear), and men are slightly more likely than women to get the cancer. Other risk factors are smoking, diabetes, and obesity.
Dr. Val: If you suspect that someone is “high risk” for pancreatic cancer, what tests should he/she have?
Dr. Lenz: Patients with a genetic predisposition for breast cancer known as BRCA are also at higher risk for pancreatic cancer. There is also a familial form of pancreatic cancer. These high risk families are being followed up with specific screening plans. However there is not a reliable test for pancreatic cancer. Imaging with CT or MRI can miss pancreatic cancer and there is no reliable blood marker. The most common used is CA 19-9, which can be used for monitoring and diagnosis but is not elevated in all patients.
Dr. Val: What if the cancer is caught very early? Does that increase likelihood of survival?
Dr. Lenz: Absolutely. The best chance of survival is when the cancer is limited to the pancreas, and is surgically removed before it reaches a size of 3 centimeters. There are certainly people who have been cured this way, but unfortunately it’s very rare to catch the cancer at such an early stage since it usually has no symptoms until it’s quite advanced.
***
There is a wonderful advocacy group for those whose lives are touched by pancreatic cancer: PanCAN. One of PanCAN’s founders, Paula Kim, is a friend of mine and was inspired to create the organization after her dad was diagnosed with pancreatic cancer in 1999. At that time there was very little advocacy for this deadly disease. PanCAN helps people with pancreatic cancer find help and support.
September 5th, 2009 by Jonathan Foulds, Ph.D. in Better Health Network, News
No Comments »

A recent research report by Professor Robert Murray (University of Manitoba) and colleagues examined whether nicotine replacement therapy (NRT) may cause cancer. The report was published in the September edition of the journal, “Nicotine and Tobacco Research”, and was based on analysis of the Lung Health Study.
The Lung Health Study recruited 5887 smokers starting November 1986, and 3923 of them were randomly selected to receive an intensive, state-of-the-art stop smoking treatment (group therapy plus nicotine gum). The participants in the original study were followed for 5 years, and 3320 were included in a longer study focusing on lung cancer for another 7.5 years.
The study presents one of the best opportunities of measuring the known exposure to either smoking, or NRT, or both over a 5 year period, as this information was accurately recorded throughout the study.
The study found that 75 participants were diagnosed with lung cancer and 203 with cancer of any type during the follow-up period. Those with the largest cigarette smoke exposure during the study were significantly more likely to suffer lung cancer, but those who used a large amount of nicotine gum were not at any greater risk of suffering from lung cancer or any other cancer examined in the study.
Even though most of the participants were relatively young at enrollment (just under 50) and so had relatively low risk over the immediately following years, around 3.2% of the heaviest smokers developed lung cancer, as opposed to half that proportion in those smoking less. But the amount of use of NRT during the study was not associated with getting cancer.
The results of this study are consistent with the vast majority of human studies, in that they do not find any convincing evidence to suggest that NRT causes cancer.
Murray RP, Connett JE, Zapawa LM. Does nicotine replacement therapy causecancer? Evidence from the Lung Health Study. Nicotine Tob Res. 2009 Sep;11(9):1076-82. Epub 2009 Jul 1.
This post, Does Nicotine Replacement Therapy (NRT) Cause Cancer?, was originally published on
Healthine.com by Jonathan Foulds, Ph.D..
 This morning, I once again get to join in with a group of noted journalists, authors, educators, and all-around people-who-do-things-I-can’t for the annual advisory board meeting of the M.S. in Medical and Science Journalism Program at the University of North Carolina at Chapel Hill’s School of Journalism and Mass Communication.
This morning, I once again get to join in with a group of noted journalists, authors, educators, and all-around people-who-do-things-I-can’t for the annual advisory board meeting of the M.S. in Medical and Science Journalism Program at the University of North Carolina at Chapel Hill’s School of Journalism and Mass Communication.