October 13th, 2010 by SteveSimmonsMD in Better Health Network, Opinion, Primary Care Wednesdays, True Stories
No Comments »
The famous late 19th and early 20th century physician, Sir William Osler, said that “a physician who treats himself has a fool for a patient.” How would he have felt about patients diagnosing and treating themselves? Would he have written in support of the Journal of Participatory Medicine or against it? I also wonder how he would have practiced medicine in the “information age” when many of our patients present with a diagnosis already made, right or wrong.
I recognize that bringing Dr. Osler into a discussion set in the information age is, perhaps, anachronistic. Yet I believe he still has something to teach the 21st century on the topic of patient participation. When he advised that “the first duty of the physician is to educate the masses not to take medicine,” he offered one of the earliest lessons on a physician’s role as educator.
He also said: “The great physician would treat the patient with the disease while the good physician would treat the disease.” For me, this marches lock-step with the reality of today’s patient as consumer and active participant in the doctor-patient relationship. Simply put, it is impossible to separate the patient from a pre-conceived and often well-researched opinion — correct or not. So to treat the “patient with the disease” requires me to think of my patient as an intellectual partner. Read more »
October 12th, 2010 by DrRob in Better Health Network, Opinion, Uncategorized
No Comments »

What is a patient? What do they do? What’s their role in the doctor’s office? Are they chassis on a conveyor belt? Are they puzzles for doctors to solve? Are they diseases? Are they demographics? Are they a repository for applied science?
Or are they consumers? Are they paying customers? Are they the ones in charge? Are they employing physicians for their own needs?
It depends. It depends on the situation. It depends on perspective.
Some physicians are very offended when the “consumer” and “customer” labels are applied to patients. They see this as the industrialization of healthcare. We are no longer professionals, we are made into “providers” — sort of smart vending-machine made out of flesh.
Patients, on the other hand, get offended when doctors forget who pays the bill. They see the exam room as a right, not a privilege. They think they should be the most important person in the exam room, being treated with respect rather than having to bow at the altar of doctor knowledge.
Who’s right? It depends. Read more »
*This blog post was originally published at Musings of a Distractible Mind*
October 12th, 2010 by KevinMD in Better Health Network, Health Policy, News, Opinion, Research
No Comments »

One of the supposed strengths of electronic medical records is better tracking of test data. In theory, when using more sophisticated digital systems, doctors can better follow the mountains of test results that they encounter daily.
But a recent study, as written in the WSJ Health Blog, says otherwise. Apparently, a study performed in 2007 found:
VA doctors failed to acknowledge receipt of 368 electronically transmitted alerts about abnormal imaging tests, or one third of the total, during the study period. In 4% of the cases, imaging-test results hadn’t been followed up on four weeks after the test was done. Another study, published in March in the American Journal of Medicine, showed only 10.2% of abnormal lab test results were unacknowledged, but timely follow-up was lacking in 6.8% of cases.
Consider that the VA has what is considered the pinnacle of electronic systems — their unified, VistA program that permeates all their hospitals and clinics. Apparently the problem is one of alert overload:
Hardeep Singh, chief of the health policy and quality program at the Houston VA’s health and policy research center, led both studies. He tells the Health Blog that doctors now receive so many electronic alerts and reminders — as many as 50 each day — that the important ones can get lost in the shuffle.
This is not unlike the alarm fatigue issue that I recently wrote about. Too much data — whether it is written or on the screen — can overwhelm physicians and potentially place patients at harm. Curating test results by prioritizing abnormals will really be the true power of electronic test reporting.
*This blog post was originally published at KevinMD.com*
October 12th, 2010 by Medgadget in Better Health Network, News, Research
No Comments »

A new sensor developed at Stony Brook University may become a clinically useful tool for detecting disease biomarkers in breath. The nanoprobe-based technology is currently able to detect acetone, but should be modifiable to spot other compounds.
From the study abstract:
This paper describes a sensor nanotechnology suitable for non-invasive monitoring of a signaling gas, such as acetone, in exhaled breath. This is a nanomedicine tool comprised of a selective acetone nanoprobe working on the principle of ferroelectric poling sensing, and a microelectronics circuit for comparing the actual sensor signal to a predetermined threshold value, displaying the result using LED signals. This on/off type non-invasive diagnostics platform technology is based on nanotechnology, gives a fast response, it is simple to operate and inexpensive to manufacture, and may truly revolutionize personalized medicine.
Full story: New Sensor Nanotechnology Developed by Stony Brook University Researchers Simplifies Disease Detection…
Abstract in Sensor Letters: Nanosensor Device for Breath Acetone Detection
*This blog post was originally published at Medgadget*
October 11th, 2010 by Shadowfax in Better Health Network, Health Policy, Opinion, Research
No Comments »

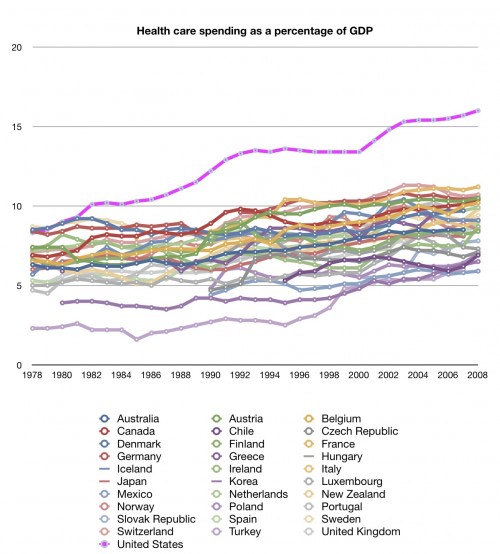
Aaron Carroll over at The Incidental Economist has been running an excellent series on healthcare spending in the U.S. and how much more we spend than the rest of the world on a per capita basis, as a percentage of GDP, and by category. It’s an excellent series and I wholly recommend it. Summary graph:
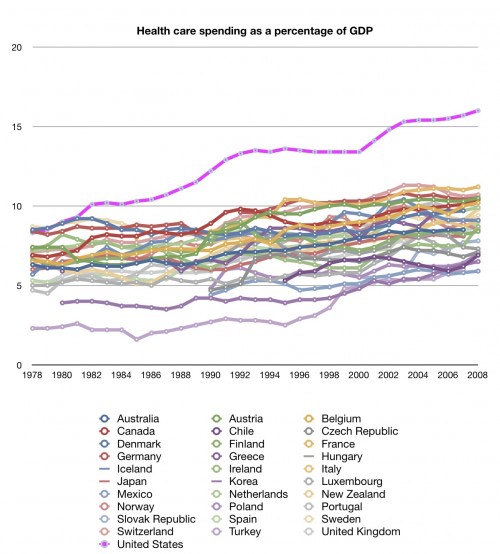
Hint: the U.S. is the lavender-ish line on top. As he says, is there anything about this graph that isn’t concerning? Read more »
*This blog post was originally published at Movin' Meat*