January 19th, 2011 by GruntDoc in Health Policy, Opinion
No Comments »

 Via an article entitled “Proposed Law Would Ban Docs From Asking If Patient Owns Gun” from First Coast News:
Via an article entitled “Proposed Law Would Ban Docs From Asking If Patient Owns Gun” from First Coast News:
TALLAHASSEE, Fla. — A state lawmaker has filed a bill that would ban doctors from asking their patients if they have a gun in the home.
Rep. Jason Brodeur, R-Sanford, said he has heard of a number of cases in which doctors asked their patients that question, which he thinks should be off limits.
“What we don’t want to do is have law-abiding firearm owners worried that the information is going to be recorded and then sent to their insurance company,” he said. “If they’re on Medicaid maybe it’s sent to the government. If the overreaching federal government actually takes over health care, they’re worried that Washington, D.C. is going to know whether or not they own a gun and so this is really just a privacy protection.”
Under the legislation, a doctor could face a fine of up to $5 million or be sent to prison for up to five years for asking about guns in the home.
I understand the stated intent as recorded in this news item: Gun ownership is being recorded, lots of things are reported to insurance companies and the government, and this bill is an attempt to keep this information out of those circles, at least as obtained in a doctors’ office where people still believe what they say is between them and their doctor. It should be, but lots of things should be absolute that aren’t. Read more »
*This blog post was originally published at GruntDoc*
December 2nd, 2010 by DrWes in Better Health Network, Health Policy, News, Opinion, Research
No Comments »

Imagine having a medical device that is being tested in multiple centers, but one doctor thinks the device has problems. He says so at a national conference despite glowing reviews by others. Should the company sue the doctor for liable and remove him from their investigative panel?
Today, it seems that might not be such a good idea. This is, in fact, what NMT Medical did regarding comments made by Peter Wilmshurst, M.D. regarding NMT’s patent foramen ovale (PFO) closure device called Starflex:
NMT sued Dr. Wilmshurst for libel after he criticized its research at a US cardiology conference in 2007. The doctor vowed to take the case to trial in order to defend scientists’ rights to free academic debate.
The company threatened Dr. Wilmshurst with libel a second time for subsequent comments he made about the case on BBC Radio 4’s Today programme. Read more »
*This blog post was originally published at Dr. Wes*
October 11th, 2010 by GruntDoc in Better Health Network, Health Policy, News, Opinion
No Comments »

According to the Standard of Care Project at EP Monthly:
The Power of Agreement
We can stop baseless malpractice suits before they get started. How? By having a majority of practicing emergency physicians go on record as to the baseline “standard of care,” beneath which is negligence.
This has been rolling for a while, and I’ve been late to blog it. That does not in any way mean I’m not 100 percent FOR it.
The idea is beautifully simple: The standard of care in emergency medicine (EM) should be set by practicing EM physicians, not case-by case in courts before lay juries with battling experts. (AAEM had the “remarkable testimony” series as a retrospective attempt to shame “experts” who gave, well, remarkable statements under oath, which to date has two cases in it.)
This has the very real advantage of being a clear, concise peer statement that this is/is not the standard of care.
I voted (while at ACEP). If you’re an emergency physician (and you have to cough up some information to determine your bona-fides before you can vote), go to the Standard of Care Project and cast your vote. They’ve set the bar at 30,000 votes, which is ambitious. It’s also worth it.
*This blog post was originally published at GruntDoc*
July 7th, 2010 by Toni Brayer, M.D. in Better Health Network, Health Policy, News, Opinion, True Stories
No Comments »

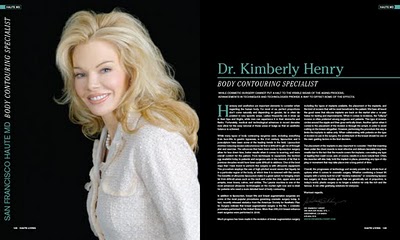 I must say I think Dr. Kimberly Henry, cosmetic surgeon, has made a big professional mistake. She has filed a lawsuit to stop online reviewers from badmouthing her on the Internet. She is seeking injunctions against at least 12 reviewers from sites such as Yelp.com and DoctorScorecard.com. Dr. Henry claims libel and defamation, invasion of privacy and interference with prospective economic advantage and is seeking $1million in general damages and $1million in special damages, etc.
I must say I think Dr. Kimberly Henry, cosmetic surgeon, has made a big professional mistake. She has filed a lawsuit to stop online reviewers from badmouthing her on the Internet. She is seeking injunctions against at least 12 reviewers from sites such as Yelp.com and DoctorScorecard.com. Dr. Henry claims libel and defamation, invasion of privacy and interference with prospective economic advantage and is seeking $1million in general damages and $1million in special damages, etc.
Now I don’t know Dr. Henry nor do I know of her plastic surgery technique. I don’t know who the disgruntled patients are or if they are unfairly targeting her. What I do know is that the Internet is here to stay and there’s no place to hide if you don’t provide excellent customer service. Read more »
*This blog post was originally published at EverythingHealth*
July 5th, 2010 by KevinMD in Better Health Network, Health Policy, News, Opinion, Research
No Comments »

Emergency physicians are in a dilemma. Risk missing a diagnosis and be sued, or be criticized for overtesting.
Regular readers of this blog, along with many other physicians’ blogs, are familiar with the difficult choices facing doctors in the emergency department.
The Associated Press, continuing its excellent series on overtesting, discusses how lawsuit fears is a leading driver of unnecessary tests. Consider chest pain, one of the most common presenting symptoms in the ER:
Patients with suspected heart attacks often get the range of what the ER offers, from multiple blood tests that can quickly add up in cost, to X-rays and EKGs, to costly CT scans, which are becoming routine in some hospital ERs for diagnosing heart attacks …
… and the battery of testing may be paying off: A few decades ago insurance statistics showed that about 5 percent of heart attacks were missed in the emergency room. Now it’s well under 1 percent, said Dr. Robert Bitterman, head of the American College of Emergency Physicians’ medical-legal committee.
“But you still get sued if you miss them,” Bitterman added.
The American Medical Association’s idea of providing malpractice protection if doctors follow standardized, evidence-based guidelines makes sense in these cases. Furthermore, it can also help reduce the significant practice variation that health reformers continually focus on. Read more »
*This blog post was originally published at KevinMD.com*
Via an article entitled “Proposed Law Would Ban Docs From Asking If Patient Owns Gun” from First Coast News:





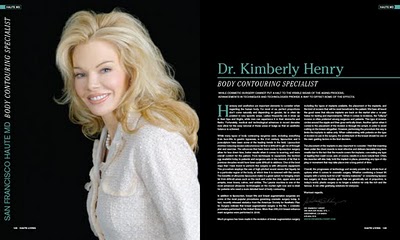 I must say I think Dr. Kimberly Henry, cosmetic surgeon, has made a big professional mistake. She has filed a lawsuit to stop online reviewers from badmouthing her on the Internet. She is seeking injunctions against at least 12 reviewers from sites such as Yelp.com and DoctorScorecard.com. Dr. Henry claims libel and defamation, invasion of privacy and interference with prospective economic advantage and is seeking $1million in general damages and $1million in special damages, etc.
I must say I think Dr. Kimberly Henry, cosmetic surgeon, has made a big professional mistake. She has filed a lawsuit to stop online reviewers from badmouthing her on the Internet. She is seeking injunctions against at least 12 reviewers from sites such as Yelp.com and DoctorScorecard.com. Dr. Henry claims libel and defamation, invasion of privacy and interference with prospective economic advantage and is seeking $1million in general damages and $1million in special damages, etc.








