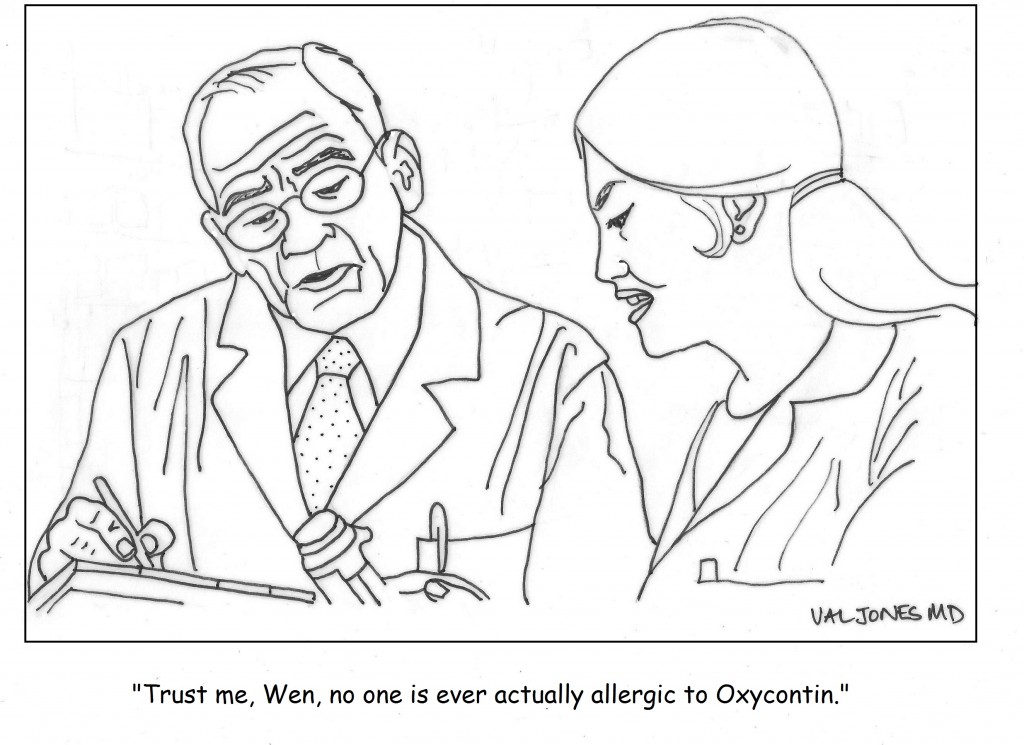
Cartoon: America’s Problem With Pain Meds

This is a guest post from Dr. Mary Lynn McPherson.
**********
FDA Restricts Acetaminophen In Popular Pain Medications
The Food and Drug Administration (FDA) made an announcement yesterday that affects one of the most common pain medications on the market, and as a consequence may affect countless numbers of the 75 million Americans who experience chronic pain (for perspective, that’s more than the number of people suffering from cancer, heart disease and diabetes combined.) The FDA has asked manufacturers of popular prescription pain medications like Vicodin or Percocet to limit the amount of acetaminophen (also known as Tylenol, or APAP) used in these drugs to no more than 325 milligrams per tablet — the equivalent of one regular-strength Tylenol tablet.
The move came because research has shown that acetaminophen can cause liver damage when taken in higher than recommended doses. The problem is that many over-the-counter medications ALSO contain acetaminophen, and patients may take one or more of these common products (like Tylenol) to reduce their fever or get rid of a headache along with their prescription pain relievers.
Before you know it, you could be taking more than the maximum daily dose of acetaminophen which is 4,000 milligrams. I go out of my way to advise people I work with of this warning, but not everyone takes time to talk to the pharmacist and not all pharmacists make themselves readily available. That is why it is critically important that you talk to your pharmacist to make sure that you are not taking more than this amount. The pharmacist is the last stop between you and medication misuse — you could be taking a medication that contains acetaminophen and not even know it. Read more »
This is a guest post from Dr. Mary Lynn McPherson.
**********
Rescuing Patients On Darvon Or Darvocet With Zero Tolerance For Pain
On November 19, 2010 the Food and Drug Administration (FDA) called for a halt in the use of the popular opioid pain relievers Darvocet and Darvon. These products contain the opioid propoxyphene, and it has been used to treat mild to moderate pain for over 50 years. However, concerns have long been raised about the effectiveness of this drug, and the risk of death (accidental and suicide). Darvon and Darvocet were banned in Britain in 2005, followed by the European Union in 2009. Over the past 30 years, the FDA has received numerous petitions to take these drugs off the U.S. market.
Research has shown that Darvon and Darvocet are no more effective for treating moderate pain than over the counter drugs like acetaminophen, aspirin or ibuprofen. Unfortunately, Darvon and Darvocet cause a lot more side effects such as dizziness, drowsiness, nausea and vomiting, hallucinations and constipation (all pretty typical of opioids used to treat pain). But, the side effects don’t stop there. The data is in, and it’s not a pretty picture. A recent study requested by the FDA showed that when used at the recommended doses, Darvon and Darvocet cause significant changes in the electrical activity of the heart, which can lead to a fatal irregularity in your heartbeat, even after only short-term use.
Among those advocating for the removal of these drugs from the market were pharmacists. The American Society of Health-System Pharmacists approved a policy in 2007 advocating for the withdrawal of Darvon and Darvocet from the U.S. market, and recently testified at the FDA Advisory Committee to this effect. As an often overlooked member of the medical team, pharmacists have a vital role to play in providing safe and effective treatments. We serve as the last line of defense against improper or unwise prescribing of drugs — especially those for pain. We are drug experts, and we can help patients and doctors switch from Darvon or Darvocet to safer and more effective treatments. Read more »
Every day in the emergency department I am confronted by pain. In fact, the treatment of pain is one of the most important skills emergency physicians, indeed all physicians, possess.
For instance, I recently cared for a child with sickle cell disease who was having a pain crisis which involved severe leg pain. His life is one of frequent, intense pain. I gently, and repeatedly, treated his pain with morphine until he had relief. I see hip fractures; all broken bones hurt. I am thrilled to alleviate that discomfort. Pain is one of the things I can fix, if only temporarily. It makes me happy to see the relaxed face of a man or woman with a kidney stone or migraine, who suddenly smiles and says “thanks!”
But pain is also the source of so much subterfuge. Emergency department are full of individuals who use controlled substances for recreation. I know because they have pain that is entirely unverifiable. They have terrible right flank pain with no gall-bladder, no pancreatitis, no kidney stone (documented by CT), no pneumonia or rash. They have nothing to cause the pain. And yet, dose after dose of narcotic later, snoring in their ER stretcher, they look up at me with hazy eyes and say, thickly, “Cann I gettt somethinn elsss for paaiin…it hurtssss so…bad. zzzz. Itzzz a tennn.”
So I began to wonder about science and the pain scale. Read more »
*This blog post was originally published at edwinleap.com*

Migraine.
Three days.
Out of pain medication and vomiting so you wouldn’t keep it down, anyway.
Agony.
Emergency department.
*****
You’re in luck – no one in triage!
A bed opens up, the nurse takes you straight to a room.
Gown, blanket.
And….
Two minutes later you send your cousin out to ask how long it will be until you get your pain med.
Excuse me? Read more »
*This blog post was originally published at Emergiblog*
It’s no secret that doctors are disappointed with the way that the U.S. healthcare system is evolving. Most feel helpless about improving their work conditions or solving technical problems in patient care. Fortunately one young medical student was undeterred by the mountain of disappointment carried by his senior clinician mentors…
I am proud to be a part of the American Resident Project an initiative that promotes the writing of medical students residents and new physicians as they explore ideas for transforming American health care delivery. I recently had the opportunity to interview three of the writing fellows about how to…
Book Review: Is Empathy Learned By Faking It Till It’s Real?

I m often asked to do book reviews on my blog and I rarely agree to them. This is because it takes me a long time to read a book and then if I don t enjoy it I figure the author would rather me remain silent than publish my…
The Spirit Of The Place: Samuel Shem’s New Book May Depress You

When I was in medical school I read Samuel Shem s House Of God as a right of passage. At the time I found it to be a cynical yet eerily accurate portrayal of the underbelly of academic medicine. I gained comfort from its gallows humor and it made me…
Eat To Save Your Life: Another Half-True Diet Book

I am hesitant to review diet books because they are so often a tangled mess of fact and fiction. Teasing out their truth from falsehood is about as exhausting as delousing a long-haired elementary school student. However after being approached by the authors’ PR agency with the promise of a…