October 19th, 2011 by KennyLinMD in Health Policy, Opinion
No Comments »

The past few months have offered encouraging signs that physicians and physician organizations are belatedly recognizing the need to take an active role in controlling health care costs by emphasizing “high-value” care and minimizing the use of low-value interventions with high costs and few clinical benefits. On the heels of a best practice guideline issued by his organization, American College of Physicians Executive VP Steven Weinberger, MD recently called for making cost-consciousness and stewardship of health resources a required general competency for graduate medical education.
In light of a recently published estimate that the top 5 overused clinical activities in primary care specialties led to $6.7 billion in wasted health spending in 2009, Dr. Weinberger’s call comes none to soon. Below is an excerpt from my post on this topic from April 13, 2010. Read more »
*This blog post was originally published at Common Sense Family Doctor*
October 17th, 2011 by Dinah Miller, M.D. in News
No Comments »



U N I T E D N A T I O N S
THE SECRETARY-GENERAL—MESSAGE ON WORLD MENTAL HEALTH DAY: 10 October 2011
There is no health without mental health. Mental disorders are major contributors to illness and premature death, and are responsible for 13 percent of the global disease burden. With the global economic downturn – and associated austerity measures – the risks for mental ill-health are rising around the globe.
Poverty, unemployment, conflict and war all adversely affect mental health. In addition, the chronic, disabling nature of mental disorders often places a debilitating financial burden on individuals and households. Furthermore, individuals with mental health problems – and their families – endure stigma, discrimination and victimization, depriving them of their political and civil rights and constraining their ability to participate in the public life of their societies.
Resources allocated for mental health by governments and civil society are Read more »
*This blog post was originally published at Shrink Rap*
October 16th, 2011 by Elaine Schattner, M.D. in Research
No Comments »

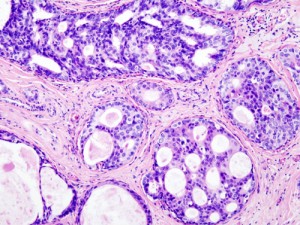
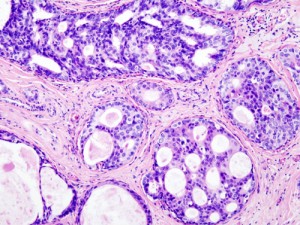
Ductal Carcinoma in Situ (DCIS) in the breast, histopathology w/ hematoxylin & eosin stain, Wiki-Commons image
More, a magazine “for women of style & substance,” has an unusually thorough, now-available article by Nancy F. Smith in its September issue on A Breast Cancer You May Not Need to Treat.
The article’s subject is DCIS (Ductal Carcinoma in Situ). This non-invasive, “Stage 0” malignancy of the breast has shot up in reported incidence over the past two decades. It’s one of the so-called slow-growing tumors detected by mammography; a woman can have DCIS without a mass or invasive breast cancer.
While some people with this diagnosis choose to have surgery, radiation or hormonal treatments, others opt for a watchful waiting strategy. The article quotes several physicians, including oncologists, who consider Read more »
*This blog post was originally published at Medical Lessons*
October 16th, 2011 by ChristopherChangMD in Opinion
No Comments »

 Over the years, I have found that patients can be loosely grouped into 4 different types. Nothing particularly wrong with any type, but it does help me to approach patients appropriately if I can get a sense of what type they are.
Over the years, I have found that patients can be loosely grouped into 4 different types. Nothing particularly wrong with any type, but it does help me to approach patients appropriately if I can get a sense of what type they are.
The four types are:
Type A: If a surgery can “fix” or “cure” me such that I won’t have to take medications every day of my life, than let’s do it.
Type B: I will never consider surgery unless it is a life-threatening situation. If a medicine can help, why do it???
Type C: I will consider surgery only as a last resort when all else fails.
Type D: Read more »
*This blog post was originally published at Fauquier ENT Blog*
October 15th, 2011 by AndrewSchorr in Opinion, True Stories
No Comments »

It’s too young to die at age 56. It’s too young to die when you have four children and a wife. It’s too young to die when you have led one of the most successful technology companies ever. It’s too young to die when you are very rich, have so much more to do and to give back. But pancreatic cancer doesn’t care. This time, again, one of our most deadly cancers won.
Medicines, nutrition, surgery, liver transplant, apparently Steve Jobs, celebrated CEO of Apple, tried them all. But, as I wrote in a recent blog, continuing was just too much. To be sure, Jobs did not have the most common type of cancer in his pancreas. His was a neuroendocrine tumor and life expectancy can be longer. But, as has been noted widely in the media, Steve Jobs came to know that his mortality clock was ticking. His eight year-survival was probably what he knew he was facing all along. Read more »
*This blog post was originally published at Andrew's Blog*








 Over the years, I have found that patients can be loosely grouped into 4 different types. Nothing particularly wrong with any type, but it does help me to approach patients appropriately if I can get a sense of what type they are.
Over the years, I have found that patients can be loosely grouped into 4 different types. Nothing particularly wrong with any type, but it does help me to approach patients appropriately if I can get a sense of what type they are.








