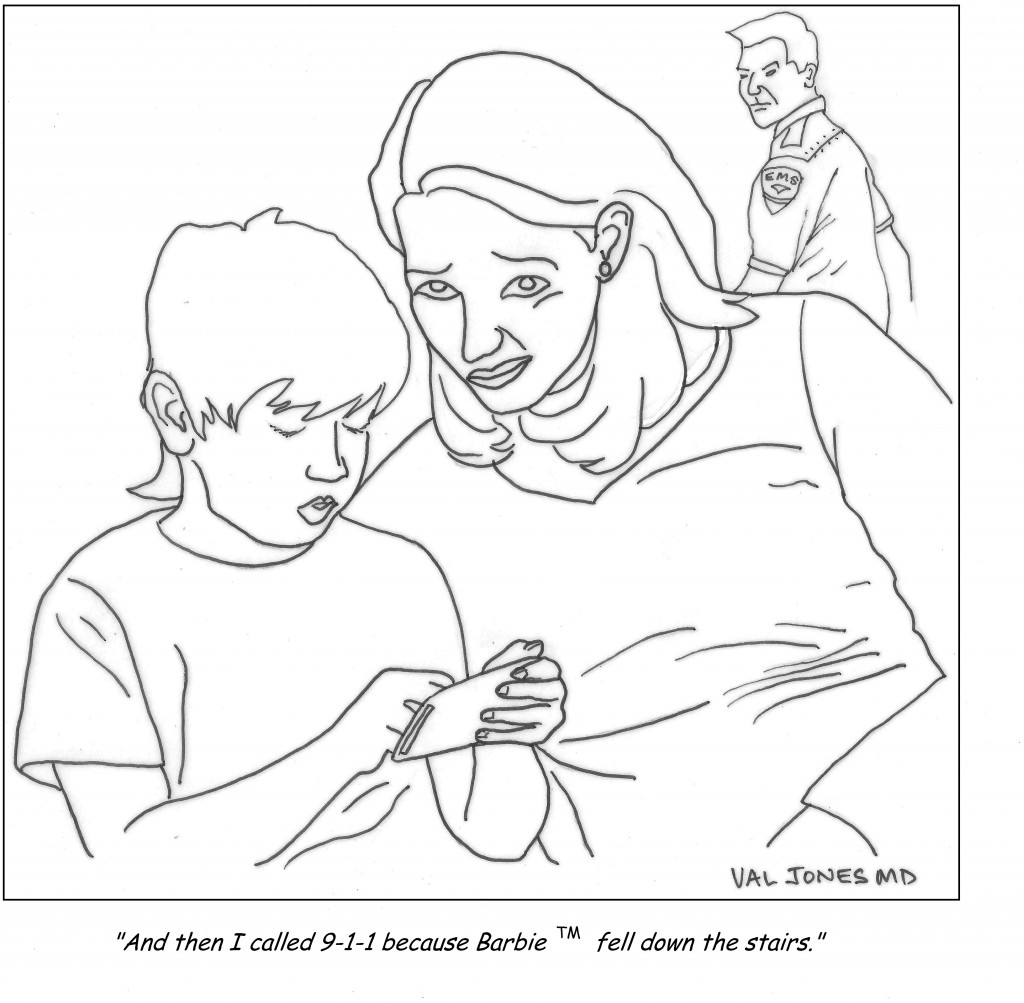
Cartoon: That Moment When You Realize Your Child Took Your Emergency Training Very Literally

The events of 9/11 will forever be engrained in our memories. The attacks on the twin towers, Pentagon, and the anthrax attacks which followed were unimaginable at the time. Ten years after these tragic events, what’s changed?

We now know that terrorist threats are ever present and that our nation must be in a constant state of vigilance in order to protect our communities. We’ve come a long way since 2001 in bolstering our nation’s ability to prepare for and respond to catastrophic events whether natural, accidental, or intentional. We are also learning more and more every day that the resources we need for the big disasters are much the same as the ones we use for everyday public health activities.
Check out my list of top 5 accomplishments in the years after the 2001 attacks: Read more »
*This blog post was originally published at Public Health Matters Blog*
 Nora misjudged the height of the stair outside the restaurant, stepped down too hard, jammed her knee and tore her meniscus. Not that we knew this at the time. All we knew then was that she was howling from the pain.
Nora misjudged the height of the stair outside the restaurant, stepped down too hard, jammed her knee and tore her meniscus. Not that we knew this at the time. All we knew then was that she was howling from the pain.
There we were on a dark, empty, wet street in lower Manhattan, not a cab in sight, with a wailing, immobile woman. What to do? Call 911? Find a cab to take her home and contact her primary care doctor for advice? Take her home, put ice on her knee, feed her Advil and call her doctor in the morning?
Sometimes it is clear that the only response to a health crisis is to call 911 and head for the emergency department (ED). But in this case – and in so many others we encounter with our kids, our parents, our co-workers and on the street – the course of action is less obvious, while the demand for some action is urgent.
 The question “which action?” has become more complicated of late because:
The question “which action?” has become more complicated of late because:
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
 I’m sure you’ve seen them on medical blogs: Disclaimers that remind readers to call 911 in the event of emergency.
I’m sure you’ve seen them on medical blogs: Disclaimers that remind readers to call 911 in the event of emergency.
But is someone choking on a hot dog really going to dial up KevinMD or SeattleMamaDoc for help? Does anyone really believe that 33 charts is the place to deal with your acute airway obstruction when you have a just a couple of minutes to live?
Here’s my theory: I suspect that the first attorney who came up with the 911 disclaimer did so as some sort of perverse joke. And rather than seek the input of their own lawyers, all those who followed simply copied the this original language believing it to be judicious and most conservative. Now it’s the longest running gag in legal history. Read more »
*This blog post was originally published at 33 Charts*
This is so wrong.
You can’t make this stuff up.
It seems an emergency department in Memphis, Tennessee is now taking online reservations for their services. Yes, you heard that right, you can now hop online and select the time you would like to be seen for your “emergency”. Just pay $15.00 and you can give your chief complaint, your medical history and your list of medications ahead of time, saving you time and trouble when you pop in with your pesky problem!
What if the problem is serious?
The computer won’t let you register and flashes a “Call 911″ sign at you.
But wait! There’s more!
If you are not seen within 15 minutes of your scheduled time, you money is cheerfully refunded!
I’m not kidding. Read more »
*This blog post was originally published at Emergiblog*
It’s no secret that doctors are disappointed with the way that the U.S. healthcare system is evolving. Most feel helpless about improving their work conditions or solving technical problems in patient care. Fortunately one young medical student was undeterred by the mountain of disappointment carried by his senior clinician mentors…
I am proud to be a part of the American Resident Project an initiative that promotes the writing of medical students residents and new physicians as they explore ideas for transforming American health care delivery. I recently had the opportunity to interview three of the writing fellows about how to…
Book Review: Is Empathy Learned By Faking It Till It’s Real?

I m often asked to do book reviews on my blog and I rarely agree to them. This is because it takes me a long time to read a book and then if I don t enjoy it I figure the author would rather me remain silent than publish my…
The Spirit Of The Place: Samuel Shem’s New Book May Depress You

When I was in medical school I read Samuel Shem s House Of God as a right of passage. At the time I found it to be a cynical yet eerily accurate portrayal of the underbelly of academic medicine. I gained comfort from its gallows humor and it made me…
Eat To Save Your Life: Another Half-True Diet Book

I am hesitant to review diet books because they are so often a tangled mess of fact and fiction. Teasing out their truth from falsehood is about as exhausting as delousing a long-haired elementary school student. However after being approached by the authors’ PR agency with the promise of a…