November 30th, 2012 by Dr. Val Jones in Book Reviews
No Comments »
 I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.
I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.
Just two months ago my fiancé sent me a “must read” article from the Wall Street Journal. It was Marty’s provocative piece, “How To Stop Hospitals From Killing Us.” The article was an excellent primer for his book, “Unaccountable: What Hospitals Won’t Tell You And How Transparency Can Revolutionize Health Care” which I highly recommend (holiday gifts, anyone?)
Unaccountable is both horrifying and oddly optimistic. Marty describes case after case of medical errors, lapses in judgment, and near misses in the surgical suite. He exposes the cultural foibles of the medical and hospital hierarchy, leaving no dirty stone unturned. Surgical delinquents such as Dr. Hodad (“hands-of-death-and-destruction”) are presented with detached accuracy, along with a clear list of reasons why the system fails to prevent the Hodads of the world from operating.
From the micro (individual physician mistakes) to the macro (trends in hospital safety breakdowns), Marty turns to survey data to make sense of the shortcomings. Interestingly, hospital “culture” (rated by its own employees) is the most predictive of overall hospital safety performance. Detailed record keeping of surgical complication rates correlates strongly with how employees rate their hospital on three simple questions:
1. Would you have your operation at the hospital in which you work?
2. Do you feel comfortable speaking up when you have a safety concern?
3. Does the teamwork here promote doing what’s right for the patient?
Marty’s conclusion that culture is the defining factor in patient safety and satisfaction ratings is both accurate and squishy. It’s difficult to create a reproducible template for a healthy work culture, and yet good culture is the basis for the success of hospitals such as the Mayo Clinic. Individual hospitals, like individual surgeons, have different personalities and temperaments. Raising them to be upstanding citizens involves a combination of good parenting and good luck.
Because I think Marty is absolutely right about culture as the foundation for safe and effective care, I think he’s also overly optimistic about the potential success of strategies to reproduce caring hospital cultures. By his own admission, not even the Mayo Clinic “mother ship” in Rochester, MN, has been able to create the exact level of quality care in its sister hospitals in Scottsdale, AZ, and Jacksonville, FL. So how can we dramatically improve patient care on a national level? Marty suggests that we need to find ways to force hospitals to become more transparent in order to revolutionize healthcare. His ideas include:
1. Mandatory hospital public reporting of patient re-admissions, complication rates, and never events.
2. Adoption of check lists by surgical teams to reduce errors.
3. Installation of video cameras throughout hospital floors and surgical suites so that staff behaviors can be monitored more effectively (e.g. to enforce hand washing or identify surgeons who have high error rates).
4. Accessible and transferable medical records that put patients at the center of their documentation.
While these ideas have merit, I believe they will fall short of achieving our ultimate goals. In my view, a culture of accountability is not the same as a culture of caring. Adopting certain “Big Brother” (cf. #3 above) strategies to pressure staff to behave/perform appropriately is only going to force the Hodads underground. We need staff to genuinely care enough about their patients to gang up on the Hodads and kick them out of the hospital for good. Caring doesn’t happen at a national level, it is personal and local. That’s why individual hospitals must develop their unique cultures for themselves, with progress measured by responses to those staff questions about whether or not they’d want to be cared for at their own institution.
I agree with Marty that hospital data transparency might be the best antiseptic we have to scrub the underbelly of medicine, though the ultimate success of our procedures will always be culture and surgeon-dependent. And that’s something you can’t regulate from Washington.
***
Marty’s book is available for purchase at Amazon.com.
Check out your local hospital safety scores from LeapFrogGroup.
November 28th, 2012 by Dr. Val Jones in Health Policy, Opinion, Primary Care Wednesdays
No Comments »
 Animal research has shown that the best way to get a rat to press a pellet-producing lever is to set the mechanism so that it doesn’t always release a pellet with each push. The unpredictability (or scarcity) of the reward causes the rat to seek it with more fervor. Casino owners are well aware of this phenomenon, gaming our brain’s natural wiring so that our occasional wins drive us to lose more than we would if our winning had a predictable pattern.
Animal research has shown that the best way to get a rat to press a pellet-producing lever is to set the mechanism so that it doesn’t always release a pellet with each push. The unpredictability (or scarcity) of the reward causes the rat to seek it with more fervor. Casino owners are well aware of this phenomenon, gaming our brain’s natural wiring so that our occasional wins drive us to lose more than we would if our winning had a predictable pattern.
I believe that the same principle is at work in physician reimbursement. Although most patients don’t realize this, physicians aren’t always paid for the work they do, and they are paid wildly different rates depending on how they code an encounter or procedure. After several health insurance denials of payment for legitimate work, physicians look for ways to offset their losses. Those may include changing the coding of their procedures to enhance the rate of reimbursement, exaggerating the complexity of an encounter, or (less commonly) billing for things they didn’t do. Because of the perceived injustice in a system that randomly denies payment for legitimate work, the physician feels less morally concerned about her over billing and coding foibles.
And so a vicious cycle of reimbursement deprivation, followed by fraud and abuse, becomes the norm in the U.S. healthcare system. Payers say that physicians are greedy and unethical, and physicians say that payers deny reimbursement unfairly and pay rates that are too low to be sustainable. The government’s response is to hire a cadre of auditors to ferret out physician fraud while cutting reimbursement to physicians further. This is similar to reducing the rate of pellet release to the rats in the Skinner boxes, while randomly electrocuting them through the metal flooring. The result will be that rats will work harder to find work-arounds to get their pellets, including gathering together into larger groups to share pellets. This is occurring more and more commonly as solo practitioners are joining hospitals or large group practices to make ends meet.
But we need to realize a few things about the “Skinner box healthcare system:”
1. Rats are not evil because they press levers manically when there is a scarcity of pellets. Physicians are not evil when they look for ways to make up lost revenue. While fraud and abuse are always wrong, it is not surprising that they are flourishing in an environment of decreasing reimbursement and increasing health insurance payment denials. If we want to address fraud and abuse, we need to understand why it’s happening so that our “solutions” (i.e. hiring thousands more government auditors to investigate medical practices) don’t end up being as useless as shocking the rats.
2. Health insurance (whether public or private) is not evil for trying to rein in costs. Payers are in the unenviable position of having to say “no” to certain expenditures, especially if they are of marginal benefit. With rats pressing levers at faster and faster rates for smaller and smaller pellets, all manner of cost containment mechanisms are being applied. Unfortunately they are instituted randomly and in covert manners (such as coding tricks and bureaucratic red tape) which makes the rats all the more manic. Not to mention that expensive technology is advancing at a dizzying rate, and direct-to-consumer advertising drives demand for the latest and greatest robot procedure or biotech drug. Costs are skyrocketing for a number of good and bad reasons.
3. There is a way out of the Skinner box for those primary care physicians brave enough to venture out. Insurance-free practices instantly remove one’s dietary reliance on pellets, therefore eliminating the whole lever pressing game. I joined such a practice several years ago. As I have argued many times before, buying health insurance for primary care needs is like buying car insurance for your windshield wipers. It’s overkill. Paying cash for your primary care allows you to save money on monthly insurance premiums (high deductible plans cost much less per month) and frees up your physician to care for you anywhere, anytime. There is no need to go to the doctor’s office just so that they can justify billing your insurance. Pay them for their time instead (whether by phone, in-person, or at your home/place of business) and you’ll be amazed at the convenience and efficiency derived from cutting out the middle men!
Conclusion: The solution to primary care woes is to think outside the box. Patient demand is the only limiting factor in the growth of the direct-pay market. Patients need to realize that they are not limited to seeing “only the physicians on their health insurance list” – there is another world out there where doctors make house calls, solve your problems on the phone, and can take care of you via Skype anywhere in the world. Patients have the power to set physicians free from their crazy pellet-oriented existence by paying cash for their health basics while purchasing a less expensive health insurance plan to cover catastrophic events. Saving primary care physicians from dependency on the insurance model is the surest path to quality, affordable healthcare for the majority of Americans. Will you join the movement?
November 26th, 2012 by Dr. Val Jones in Health Tips, Opinion, Research
5 Comments »
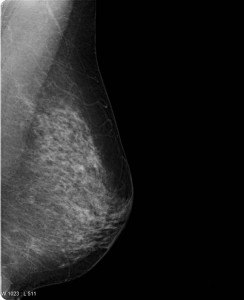
 A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
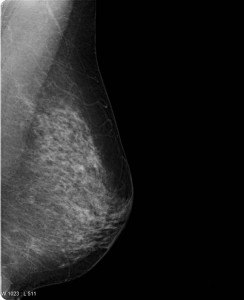
A question on most women’s minds (as they turn 40 and beyond) is whether or not they should get a screening mammogram (x-ray of the breasts). If you have found a lump in your breast or you have a family history of breast cancer the answer is yes. No need to read any further. However, for the majority of us lumpless, family-history-free women, a screening mammogram is far more likely to expose us to unnecessary follow up testing than it is to catch a tumor early. Dr. Welch explains that screening mammograms aren’t very good at identifying aggressive breast cancer early enough to make a difference in whether one lives or dies anyway. That’s very disappointing news.
Dr. Welch goes on to explain that most of the gains we’ve made in breast cancer survival have been because of improved breast cancer treatments, not because of early detection with mammograms. He estimates that every year in the U.S. 1.3 million women are “over-diagnosed” with breast cancer because of screening mammograms, subjecting women to unnecessary biopsies, surgical procedures, and further follow up studies. In the video, Dr. Welch doesn’t explain exactly what these “over diagnosed” cancers end up being exactly (Cysts? Benign calcifications? Early non-aggressive cancers that the immune system kills on its own?) But suffice it to say that they don’t contribute to the cancer death rates.
So, given the fact that you are more likely to suffer through a false alarm than to discover a cancer early (and even if you do find it early, if it’s the “bad” kind you may not survive) are you willing to undergo a screening mammogram? That’s a personal question that we each have to answer for ourselves. As time goes on, however, I suspect that the answer will be made for us since health insurance companies (whether public or private) will begin to balk at paying for tests that do more harm than good overall. I think this issue is really at the heart of the controversy (the perception of rolling back a health benefit that women currently “enjoy”). Eventually screening mammograms may become an out-of-pocket expense for women who simply prefer the peace of mind that a normal test can give – even at the risk of going through a false alarm.
That being said, it sure would be great if we could find a screening test that identifies breast cancer early – especially the aggressive kind. Perhaps a blood test will do the trick one day? At least it is comforting to know that we have made great strides on the treatment side, so that fewer women than ever before die of breast cancer. More research is needed on both the screening and treatment sides of course.
As for me, I do regular breast self exams – though because I have no family history of breast cancer I’ve opted out of screening mammograms because I feel the cost/benefit ratio is not in my favor. I certainly hope that a better screening test is developed before I face a potential diagnosis. I respect that other women will disagree with me – and I think they have the right to be screened with the only option we currently have: the mammogram. I’m not sure how long it will continue to be covered by insurance, but at a price point of about $100, most of us could still afford to pay for it out-of-pocket if desired.
The bottom line of this controversial research study is that screening mammograms don’t actually catch death-causing breast cancers early enough to alter their course. Even though it makes intuitive sense to be screened, long term observations confirm that overall, mammograms do more harm than good. So now we wait for a better test – while some of us continue with the old one (as the National Cancer Institute recommends), and others (like me) don’t bother.
***
Thanks to ePatient Dave and Susannah Fox who brought the issue to my attention on Facebook. Isn’t social media grand?
November 26th, 2012 by admin in Quackery Exposed, True Stories
No Comments »
 What did the jockey who never lost a race whisper into the horse’s ear? “Roses are red, violets are blue, Horses that lose are made into glue!” OK, so it’s a groaner. But until the advent of polyvinyl acetate (PVA) and other synthetic glues in the twentieth century, the destiny of aging horses was indeed the glue factory. The collagen extracted from their hides, connective tissues and hooves made for an ideal wood adhesive. Our word “collagen” for the group of proteins found in these tissues actually derives from the Greek “kolla” for “glue.”
What did the jockey who never lost a race whisper into the horse’s ear? “Roses are red, violets are blue, Horses that lose are made into glue!” OK, so it’s a groaner. But until the advent of polyvinyl acetate (PVA) and other synthetic glues in the twentieth century, the destiny of aging horses was indeed the glue factory. The collagen extracted from their hides, connective tissues and hooves made for an ideal wood adhesive. Our word “collagen” for the group of proteins found in these tissues actually derives from the Greek “kolla” for “glue.”
Not all aging horses were dispatched to the glue factory after their plow-pulling days came to an end. Some farmers found they could squeeze a little more profit out of the animals by assigning them another duty. They would become leech collectors! The elderly horses were driven into swampy waters only to emerge coated with the little bloodsucking worms. It seems the creatures found horses to be a particularly tasty treat! Since for many people suffering from various ailments, the little parasites were just what the doctor ordered, the harvesting of leeches made for a lucrative business.
Leeches have actually been used in medicine since they were first introduced around 1500 BC by the Indian sage Sushruta, one of the founders of the Hindu system of traditional medicine known as “Ayurveda.” That translates from the Sanskrit as “knowledge of life.” Sushruta recommended that leeches be used for skin diseases and for various musculoskeletal pains. Ancient Egyptian doctors extended the indications, treating headaches, ear infections and even hemorrhoids in this peculiar fashion. Galen, the famous Roman physician, used leeches to balance the four “humors,” namely blood, phlegm, black bile and yellow bile. Swollen, red skin, for example, was thought to be due to too much blood in the body and the answer was to have leeches slurp the excess.
Curiously, despite having no evidence for efficacy, bloodletting, either with leeches or by making an incision with a “lancet,” became part of standard medical practice for more than 2500 years! Monks, priests and barbers got into the act along with physicians. In 1799 George Washington had more than half his blood drained in ten hours, certainly hastening his demise.
Many British doctors preferred leeches, especially in areas around the mouth, ears and eyes where lancing was a tricky procedure. They even learned how to encourage a leech to bite by stimulating its appetite with sugar or alcohol. But the creatures were in short supply, and had to be imported by the millions from France, Germany, Poland and Australia where they were often caught in nets using liver as bait. Sometimes poor children earned a little extra money by wading into infested waters to emerge, like the horses, with leeches attached to their legs. A gentle tug or a pass with a flame then relaxed the bloodsucker’s grip before much damage ensued. Good thing, because leeches can be pretty nasty once they latch on. Remember Humphrey Bogart flailing about in African Queen while trying to rid himself of the little vampires?
The lack of leeches caused some physicians to explore recycling techniques. Usually a single leech becomes satiated after filling up on about 15 milliliters of blood and then falls off. But then if it is plunked into salt water, it will disgorge the blood and is soon ready for another round. A German physician even developed a technique to encourage continued sucking by making an incision in the leech’s abdomen allowing for the ingested blood to drain out as fast as it came in. It seems the leech wasn’t much bothered by this affront to its belly and would go on sucking for hours. Amazingly, leeches were sometimes used internally. To treat swollen tonsils, a leech with a silk thread passed through its body would be lowered down the throat and withdrawn when it had finished its meal. Sometimes the creatures were even introduced into the vagina to treat various “female complaints.” The literature is vague about how this was done but one account suggests that the technique required a clever nurse.
While bloodletting as a general treatment for ailments has been drained out of the modern medicine chest, there is still work for leeches. That’s because their saliva is a complex chemical mix of pain killers and anticoagulants. Hirudin, for example, is the protein that keeps the blood flowing steadily after the initial bite is made, and is so effective that the blood will not coagulate for quite some time even after the leech falls off. Indeed, these bloodsucking aquatic worms have received approval from the U.S. Food and Drug Agency as a “medical device.”
Surgeons have been known to use leeches after reattaching ears, eyelids or fingers that have been severed, as well as after skin grafts. This has to do with the fact that arteries are easy to reconnect but veins are not. Eventually new capillaries do form to reconnect veins, but in the meantime the finger or ear fills with blood which then clots and causes problems with circulation. A leech will drain the excess blood at just the right rate and can prevent blood clot formation by injecting hirudin. This is such a potent anticoagulant that it holds hope for dissolving blood clots after a heart attack or stroke. Unfortunately hirudin is too difficult to extract from leeches but can potentially be produced through genetic engineering techniques.
Where do physicians get leeches today? No need for horses. They can order them directly from the French firm Ricarimpex. One would think that after helping to save a finger or an ear the useful little critters would be rewarded. But their destiny is death in a bucket of bleach. Not any better than ending up in a glue factory.
***
Joe Schwarcz, Ph.D., is the Director of McGill University’s Office for Science and Society and teaches a variety of courses in McGill’s Chemistry Department and in the Faculty of Medicine with emphasis on health issues, including aspects of “Alternative Medicine”. He is well known for his informative and entertaining public lectures on topics ranging from the chemistry of love to the science of aging. Using stage magic to make scientific points is one of his specialties.
November 21st, 2012 by Dr. Val Jones in Health Policy, Opinion
No Comments »
 In a recent post entitled, “The Joys Of Health Insurance Bureaucracy” I described how it took me (a physician) over three months to get one common prescription filled through my new health insurance plan. Of note, I have still been unable to enroll in the prescription refill mail order service that saves my insurer money and (ostensibly) enhances my convenience. The prescription benefits manager (PBM) has lost three of my physician’s prescriptions sent to them by fax, and as a next step have emailed me instructions to complete an online form so that they have permission to contact my physician directly (to confirm the year’s refills). Unfortunately, page one of the form requires you to fill in your drug name and match it to their database’s list before you can continue to page two. For reasons I can’t understand, my common drug is not in their database. Therefore, I am unable to comply with my insurer’s wish that I enroll in mail order prescription refills. This will further delay receipt of my medication – and probably increase my cost as I will be penalized for not opting into the “preferred” mail order refill process.
In a recent post entitled, “The Joys Of Health Insurance Bureaucracy” I described how it took me (a physician) over three months to get one common prescription filled through my new health insurance plan. Of note, I have still been unable to enroll in the prescription refill mail order service that saves my insurer money and (ostensibly) enhances my convenience. The prescription benefits manager (PBM) has lost three of my physician’s prescriptions sent to them by fax, and as a next step have emailed me instructions to complete an online form so that they have permission to contact my physician directly (to confirm the year’s refills). Unfortunately, page one of the form requires you to fill in your drug name and match it to their database’s list before you can continue to page two. For reasons I can’t understand, my common drug is not in their database. Therefore, I am unable to comply with my insurer’s wish that I enroll in mail order prescription refills. This will further delay receipt of my medication – and probably increase my cost as I will be penalized for not opting into the “preferred” mail order refill process.
Now, all of this is infuriating enough on its own, but the larger concern that I have is this: How many patients are not “compliant” with their medication regimen because of problems/delays with their health insurer or PBM? Physicians are being held accountable for their patients’ medication compliance rates, even receiving lower compensation for patients who don’t reach certain goals. This is called “pay-for-performance” and it’s meant to incentivize physicians to be more aggressive with patient follow up so that people stay healthier. But all the follow up in the world isn’t going to get patient X to take their medicine each day if their health insurer or PBM makes it impossible for them to get it in the first place. And shouldn’t there be consequences for such excessive red tape? Who is holding the insurers and PBMs accountable for their inefficiencies that prevent patients from getting their medicines in a timely manner?
Pay-for-performance assumes that physicians are the only healthcare influencers in the patient compliance cycle. I’ve learned that we only play a part in helping people stay on the best path for their health. Other key players can derail our best intentions, and it’s high time that we look at the poor performance of health insurers and PBMs as they often block (with intentional bureaucracy) our patients from getting the medicine they need. While insurers save money by having patients struggle to get their prescriptions filled, doctors are payed less when patients don’t take their medicines.
Not a great time to be a doctor or a patient… or both.
 I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.
I met Dr. Marty Makary over lunch at Founding Farmers restaurant in DC about three years ago. We had an animated conversation about hospital safety, the potential contribution of checklists to reducing medical errors, and his upcoming book about the need for more transparency in the healthcare system. Marty was well dressed and soft spoken – sincere, and human. We exchanged business cards and wished each other luck in changing the healthcare system for the better. We were two doctors tilting at windmills.

 A
A 
 In a recent post entitled, “
In a recent post entitled, “







