October 11th, 2010 by Shadowfax in Better Health Network, Health Policy, Opinion, Research
Tags: Aaron Carroll, GDP, General Medicine, Global Healthcare Spending, Healthcare Costs, Healthcare Politics, Healthcare reform, Healthcare Spending In The U.S., Healthcare Spending Worldwide, Movin' Meat, Patient Protection and Affordable Care Act, Physicians' Salaries, PPACA, Shadowfax, The Incidental Economist, U.S. Healthcare System
No Comments »

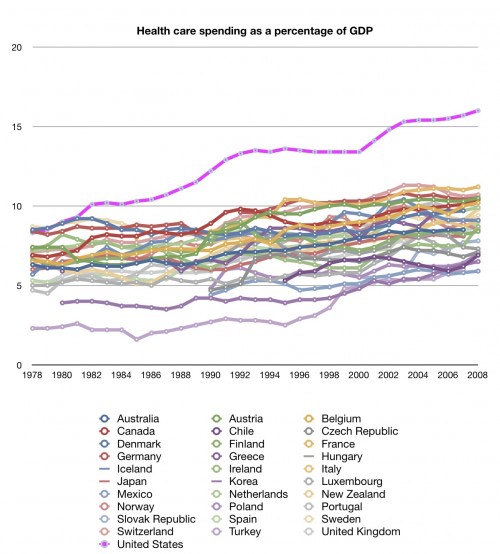
Aaron Carroll over at The Incidental Economist has been running an excellent series on healthcare spending in the U.S. and how much more we spend than the rest of the world on a per capita basis, as a percentage of GDP, and by category. It’s an excellent series and I wholly recommend it. Summary graph:
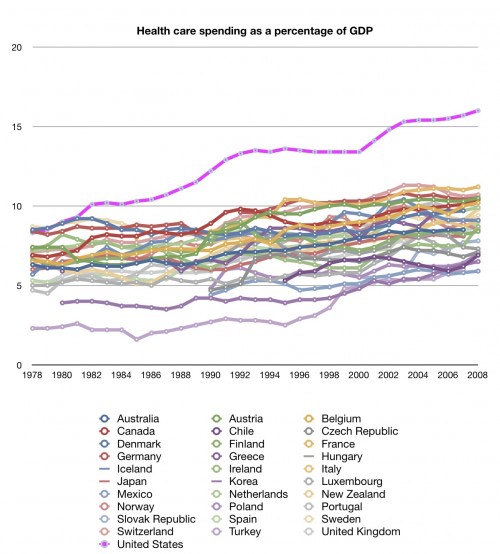
Hint: the U.S. is the lavender-ish line on top. As he says, is there anything about this graph that isn’t concerning? Read more »
*This blog post was originally published at Movin' Meat*
October 11th, 2010 by DavedeBronkart in Better Health Network, Health Policy, Opinion
Tags: 33 Charts, Dave deBronkart, Dr. Bryan Vartabedian, ePatient Dave, General Medicine, Healthcare Policy, Participatory Medicine, Patient Engagement, Patient Participation, Patients As Healthcare Consumers, Personalized Medicine, Regulate Patient Consumers
1 Comment »

Last month in Cambridge I met Twitter friend Bryan Vartabedian, M.D. (Twitter @Doctor_V) at a meeting at Vertex Pharmaceuticals. We’ll cross paths this fall on the conference speaking circuit. [Recently] on his blog he raised a rowdy, rough, but valid point: As e-patients (obviously including me) get into the business, should they/we be regulated? He said:
Will industry be required to publicly list monies used for sponsorship, travel and swag support of high profile patients in the social sphere?
Should high visibility patients who serve as stewards and advocates disavow themselves of contact with pharma just as many academic medical centers have begun?
As is often the case, I don’t have an answer. I’m just raising the questions. Smart questions. My short answer:
- Fine with me if industry discloses those payments. Nothing to hide.
- On the other hand, I think it’s nuts and counterproductive for consumers in any industry to disconnect.
Academic medical centers have tons of evidence of influence corrupting the academic processes that are at the core of (supposed) science. For patient advocates I don’t see that there’s currently a problem that would justify adding regulators, the ensuing budget impact, etc.
Besides, there’s a key difference: Academics are supposed to vet industry. It’s their job in this context. Patients, on the other hand, are the consumers — the ones the industry’s supposed to serve. Read more »
*This blog post was originally published at e-Patient Dave*
October 11th, 2010 by DavidHarlow in Better Health Network, Health Policy, News, Opinion, Research
Tags: Chilmark Research, David Harlow, Goodfellas, Google Health, HealthBlawg, Healthcare Costs, Healthcare Quality, Healthcare Status, Healthcare Wired, John Moore, mHealth, Microsoft HealthVault, Mobile Health, Mobile Health Monitoring Devices, Mobile Health Reminder Services, Price, PWC
No Comments »

Last month, PricewaterhouseCoopers (PwC) issued a report, Healthcare Unwired, examining the market for mobile health monitoring devices, reminder services, etc. among both healthcare providers and the general public. One of the big take-away points seems to be that 40% of the general public would be willing to pay for mobile health (or “mHealth”) devices or services ranging from reminders to data uploads — and the reaction by insiders is either joy (40% is good) or dismay (40% is not enough).
PwC estimated the mHealth market to be worth somewhere between $7.7 billion and $43 billion per year, based on consumers’ expressed willingness to pay. Deloitte recently issued a report on mPHRs, as well — and there is tremendous interest in this space, as discussed in John Moore’s recent post over at Chilmark Research. I agree with John’s wariness with respect to the mHealth hype — there is certainly something happening out there, but significant questions remain: What exactly is going on? Is there reason to be interested in this stuff or is it just something shiny and new? Can mHealth improve healthcare status and/or healthcare quality and/or reduce healthcare costs? Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
October 11th, 2010 by GruntDoc in Better Health Network, Health Policy, News, Opinion
Tags: AAEM, American Academy of Emergency Medicine, ED, EM, Emergency Department, Emergency Doctors, Emergency Room, EP Monthly, ER Doctors, Medical Lawsuits, Medical Malpractice, Standard Of Care Project
No Comments »

According to the Standard of Care Project at EP Monthly:
The Power of Agreement
We can stop baseless malpractice suits before they get started. How? By having a majority of practicing emergency physicians go on record as to the baseline “standard of care,” beneath which is negligence.
This has been rolling for a while, and I’ve been late to blog it. That does not in any way mean I’m not 100 percent FOR it.
The idea is beautifully simple: The standard of care in emergency medicine (EM) should be set by practicing EM physicians, not case-by case in courts before lay juries with battling experts. (AAEM had the “remarkable testimony” series as a retrospective attempt to shame “experts” who gave, well, remarkable statements under oath, which to date has two cases in it.)
This has the very real advantage of being a clear, concise peer statement that this is/is not the standard of care.
I voted (while at ACEP). If you’re an emergency physician (and you have to cough up some information to determine your bona-fides before you can vote), go to the Standard of Care Project and cast your vote. They’ve set the bar at 30,000 votes, which is ambitious. It’s also worth it.
*This blog post was originally published at GruntDoc*
October 11th, 2010 by Dinah Miller, M.D. in Better Health Network, Health Policy, Opinion
Tags: Diagnosis Criteria, Dr. Dinah Miller, Dr. Mitchell Newmark, DSM-V, Inaccurate Diagnosis, Misdiagnosis, Multiple Diagnoses, My Three Shrinks, No Clear-Cut Diagnosis, Overdiagnosis, Psychiatric Diagnosis, Psychiatry and Psychology, Shrink Rap, Wrong Diagnosis
No Comments »


 Look, he came back! Guest blogger Mitchell Newmark, M.D., put on his armor and came to blog with us again.
Look, he came back! Guest blogger Mitchell Newmark, M.D., put on his armor and came to blog with us again.
The Relative Unimportance of Diagnosis In Psychiatry
As we will soon be witness to the emergence of DSM-V, the new rule book for psychiatric diagnosis, I am reminded of all the pitfalls of diagnosis in psychiatry. In other fields of medicine, diagnosis is based primarily on etiology, with objective findings, rather than on symptoms alone, as it is in psychiatry. When you go to your internist with stomach pain, there’s an endoscopy to look for ulcers, a sonogram to look for gall stones, a blood test to look for hepatitis. But in psychiatry, there is no CT scan to check for bipolar disorder, no blood test to assess if the patient has schizophrenia, no spinal tap to check for major depression.
For the psychiatric community at large, diagnosis is important for many reasons. It helps doctors sort out patients so that clinical trials can be conducted on similar groups of patients. It enhances communication among psychiatrists when behavioral, affective and cognitive symptoms can be categorized. But for the individual patient, it is less useful. Some patients fit nicely into DSM categories, and others don’t. There are many patients who have unique combinations of symptoms across several diagnostic criteria. This leads to assigning multiple diagnoses, and confusing the treatment picture. Read more »
*This blog post was originally published at Shrink Rap*