
March 7th, 2011 by Dr. Val Jones in Health Policy, True Stories
Tags: Bureaucratic Obstacles To Practicing Medicine, Dr. Val Jones, FCVS, Federation Credentials Verification Service, Finding a Doctor in California, License To Practice Medicine, Medical Board of California, Medical Bureaucracy, Medical Credentialing, Medical License, Physician Frustration, Practicing Medicine in California
8 Comments »
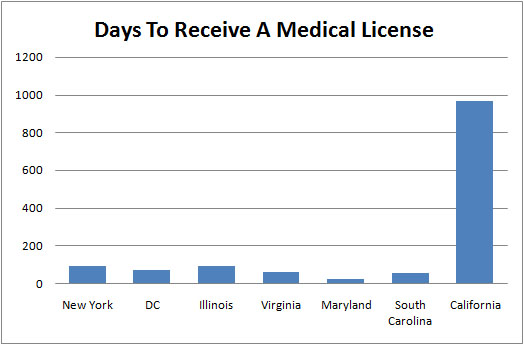
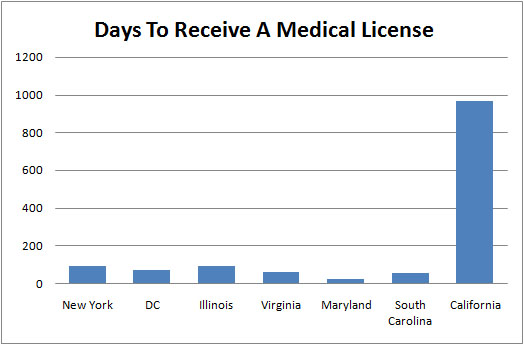
I first applied for a license to practice medicine in the state of California on July 9, 2008. I was licensed on March 3, 2011 — a whopping 967 days after they first received my application. I haven’t had a problem getting a license in any other state, and I am licensed in six of them. Just to give you a sense of how long it usually takes to process the paperwork for a medical license, Maryland completed mine in under three weeks. So what’s going on in California?
Dr. Val’s Experience
I think the best way to tell this story is with a timeline, and let the facts speak for themselves. I know this represents just one physician’s experience (namely mine), so results may vary:
July 9, 2008 – The Medical Board of California (MBC) received my licensure application and my checks for $493 (for fingerprint and processing fee) and $805 (initial licensing fee), which were cashed soon thereafter.
Sept 29, 2008 – I received a letter in the mail stating that there were four items missing from my application. Two of these four items were already included in the Federation Credentials Verification Service (FCVS) packet they had received from me. The other two items were requests for residency program directors to write letters to support the forms that they had already filled out on my behalf. I immediately requested these letters, and even though I should not have needed to send additional copies of items from the FCVS packet, I did so as well.
December 3, 2008 – I received a letter in the mail from the MBC, stating that there was an additional fee of $25 now required for physicians whose licensure applications were postmarked after December 31, 2008. This obviously didn’t relate to me, but the letter reminded me to follow up with the board to make sure that they had received the four items from the Sept 29th letter. I sent the licensing program administrator an email and left a voice message for follow-up purposes. He gave no response. Read more »
March 6th, 2011 by Edwin Leap, M.D. in Opinion, True Stories
Tags: A Doctor's Mind, Being Smarter Than Your Brain, Controlling Your Thoughts, Doctors and Decision Making, Doctors and Mental Focus, Doctors and Mental Strength, Doctors and Thought Processes, Doctors' Perspective, Doctors' Thoughts, Emergency Medicine, Emotional Health, General Medicine, Good Medical Decision Making, Good Thoughts, Healthy Mind, Heuristics, Hostage To Your Thoughts, Mental Health, Optimism, Physicians and Thought Control, Positive Thinking, Processing Thoughts, Psychology of Medicine, The Impact Of Thought
1 Comment »

 Here’s my column in the March issue of Emergency Medicine News.
Here’s my column in the March issue of Emergency Medicine News.
Second Opinion: Be Smarter Than Your Brain
“Everyone is a drug seeker. Why does everyone want to be on disability? I’m so tired of lies. Great, another lousy shift. I wonder who will die tonight? I’m so sick of suffering. I’m so weary of misery and loss. I hope this never happens to my family. I’ll probably get sued. Being sued nearly drove me crazy. This job never gets easier, only harder. I have to find something else to do; I can’t go on this way. I think I’m going crazy. I don’t have any more compassion. People hate me now.”
These are only a few of the wonderful thoughts that float through the minds of emergency physicians these days. Sure, not every physician has them. But I know our specialty, I know our colleagues, I hear from doctors around the country and I see that fear, frustration and anxiety are common themes.
Older physicians fantasize about career changes, and younger ones are often blind-sided by the hard realities of practice outside of their training programs (where their work-hours and staffing do not necessarily reflect the world beyond).
We are crushed by regulations and overwhelmed by holding patients, often put in situations where we are set squarely between the devil and the deep blue sea. “Spend more time with your patients; see them faster. Don’t let the ‘psychiatric hold’ patient escape; why are you using so much staff on psychiatric patients? See chest pain immediately; why didn’t you see the board member’s ankle injury as fast as the chest pain?”
In all of this mess of emergency medicine, we often find ourselves frustrated and bitter. But is it only because of our situations? They are admittedly daunting. But is our unhappiness merely the result of the things imposed on us? Or could it be more complex than that? Lately, I have come to wonder if our thoughts are perhaps worse enemies than even lawsuits, regulations, or satisfaction scores. Read more »
*This blog post was originally published at edwinleap.com*
March 5th, 2011 by Dr. Val Jones in True Stories
Tags: Arrhythmia, Cardiology, Cycling, Defibrillator, Errors, Exercise, Fitness, Heart Rate, Laboratory, Mix Ups, Monitor, Rapid Heart Rate, Spinning
1 Comment »
 In medicine we’re often reminded not to base our therapy solely on lab test results. Although it’s tempting to reduce patient care to a checklist of “normal” bloodwork targets, we all know that this is only a fraction of the total health picture. Today I made a mistake that brought this truism home: “Don’t treat the number, treat the patient.”
In medicine we’re often reminded not to base our therapy solely on lab test results. Although it’s tempting to reduce patient care to a checklist of “normal” bloodwork targets, we all know that this is only a fraction of the total health picture. Today I made a mistake that brought this truism home: “Don’t treat the number, treat the patient.”
I’m turning 40 this year and decided to make an ambitious fitness goal for myself — to be in better shape at 40 than I was at 30. No small feat for a person who used to be in good form a decade ago (not so much now, ahem). So, I joined a gym owned by an affable triathlete and invited her to make me her project. Let’s just say that Meredith believes that one piece of sprouted grain bread is the breakfast of champions — and with that she has me doing many hours of cardio sprints and strength training every week. I’m still alive. Barely.
Today in my endurance spinning class (an unusual form of torture where you get yelled at — I mean encouraged — on a stationary bicycle for an hour and a half in a dark room filled with high-decibel rock music and sweaty co-sufferers), I was somewhat alarmed by my heart rate. I was taught in medical school that one’s maximum heart rate is 220 minus your age. So mine should be about 180. I assumed that anything higher than that was incompatible with life.
So when I saw my heart rate monitor rise to 185 on a steep climb at maximum speed, I wondered if I might be about to die. I certainly felt physically challenged, but not quite at death’s door, so I looked around sheepishly at my nearest peer’s monitor to see if she was handling the strain any better. Nope, she was also at 185. “Gee, what a coincidence,” I thought. “We must be exactly the same fitness level.” Read more »
March 4th, 2011 by Jeffrey Benabio, M.D. in Health Tips, True Stories
Tags: Climate And Your Skin, Climate Change, Dermatology, Dr. Jeff Benabio, Eczema, Hard Water, Non-Soap Cleansers, Skin Care, Skin Moisturizer, Skin Rash, Soap
No Comments »

 Hard water is tap water that’s high in minerals such as calcium and magnesium. Hard water isn’t harmful, except the minerals prevent your soap from sudsing. Some people think that hard water is more likely to cause a rash than soft water.
Hard water is tap water that’s high in minerals such as calcium and magnesium. Hard water isn’t harmful, except the minerals prevent your soap from sudsing. Some people think that hard water is more likely to cause a rash than soft water.
Take a recent patient of mine: He moved his family to San Diego from the East Coast (good move this winter, no?) After they moved here, they noticed their skin became dry and itchy. He blamed San Diego’s notoriously hard water and installed a water softener in the main water line. It was costly, but did it improve their skin?
A recent study from the UK looked at this question: Does hard water worsen eczema? The answer was no, it doesn’t. Water hardness did not seem to have any impact on eczema, the most common skin rash.
What’s more important than the hardness of the water is the type of soap you use. True soap tends to strip the skin of its natural oils, leaving it exposed and irritated. Non-soap cleansers, of which Dove is the prototype, leave more oils on your skin, keeping it hydrated and protected.
My patient and his family didn’t get any better after installing a water softener (although he said they could drink our tap water without gagging now.) I advised him to change to a moisturizing soap and to apply moisturizer daily.
San Diego is drier than most of the country, and the low humidity can be a shock to skin accustomed to humid air. Many people who move here find they have to moisturize more often than they did back home. When they complain, I suggest they could alternatively move back to the East Coast this winter — no takers so far.
*This blog post was originally published at The Dermatology Blog*
March 4th, 2011 by Bryan Vartabedian, M.D. in Opinion, True Stories
Tags: 33 Charts, Charlene Li, Doctor Patient Relationship, Doctors and Social Media, Doctors on the Internet, Dr. Bryan Vartabedian, Facebook, General Medicine, Healthcare Professionals Online, Healthcare Social Media, Medicine and Social Media, Online Physician Conduct, Professional Behavior On The Internet, Professionalism In Healthcare, Social Health Media, Twitter
No Comments »

This week a reporter cornered me on the issue of professional behavior in the social space. How is it defined? I didn’t have an answer. But it’s something that I think about.
Perhaps there isn’t much to think about. As a “representative” of my hospital and a physician to the children in my community, how I behave in public isn’t any different than a decade ago. Social media is just another public space. Sometimes it’s easy to forget that we’re in public. When I’m wrapped up in a Twitter thread it’s easy to forget that the world is watching. But the solution is simple: Always remember that the world is watching.
On Twitter I think and behave as I do in public: Very much myself but considerate of those around me. I always think about how I might be perceived.
Here’s a better question, online or off: What is professional behavior? I have a pediatrician friend who, along with the rest of his staff, wears polo shirts and khaki shorts in the summer. The kids love it. One of my buttoned-down colleagues suggested that this type of dress is “unprofessional.” Or take a handful of physicians and ask them to review a year of my blog posts and my Twitter feed. I can assure you that some will identify elements that they find “unprofessional.” I believe I keep things above board.
This is all so subjective.
The reporter was also interested in how I separate my professional and personal identities in the online space. I’m not sure the two can be properly divided. The line is increasingly smudged. I try to keep Facebook as something of a personal space. I think it was Charlene Li who suggested that she only “friends” people she knows well enough to have over for dinner. That’s evolving as my rule as well. But independent of how I define “well enough,” Facebook is still a public space. My comments and photos can be copied to just about anywhere.
Social media has not forced the need for new standards of physician conduct. We just need to be smarter than we were before. Everyone’s watching.
*This blog post was originally published at 33 Charts*





 In medicine we’re often reminded not to base our therapy solely on lab test results. Although it’s tempting to reduce patient care to a checklist of “normal” bloodwork targets, we all know that this is only a fraction of the total health picture. Today I made a mistake that brought this truism home: “Don’t treat the number, treat the patient.”
In medicine we’re often reminded not to base our therapy solely on lab test results. Although it’s tempting to reduce patient care to a checklist of “normal” bloodwork targets, we all know that this is only a fraction of the total health picture. Today I made a mistake that brought this truism home: “Don’t treat the number, treat the patient.”









